Sleep Apnea Detection Technology: What Works and What Doesn't [2025]
I woke up gasping for air at 3 AM last Tuesday. Not from a nightmare. From actual sleep apnea—a condition where your breathing stops and starts repeatedly while you're asleep. The doctor confirmed it after a sleep study, so I decided to turn my own sleep into a test lab.
I own several sleep trackers. Fitbit. Apple Watch. Oura Ring. All of them claim to detect breathing irregularities. All of them cost between
The answer? It's complicated. Some flagged issues consistently. Others missed the problem entirely. One caught something the doctor actually cared about. And here's what surprised me most—none of them are a replacement for a real sleep study, but they're getting closer.
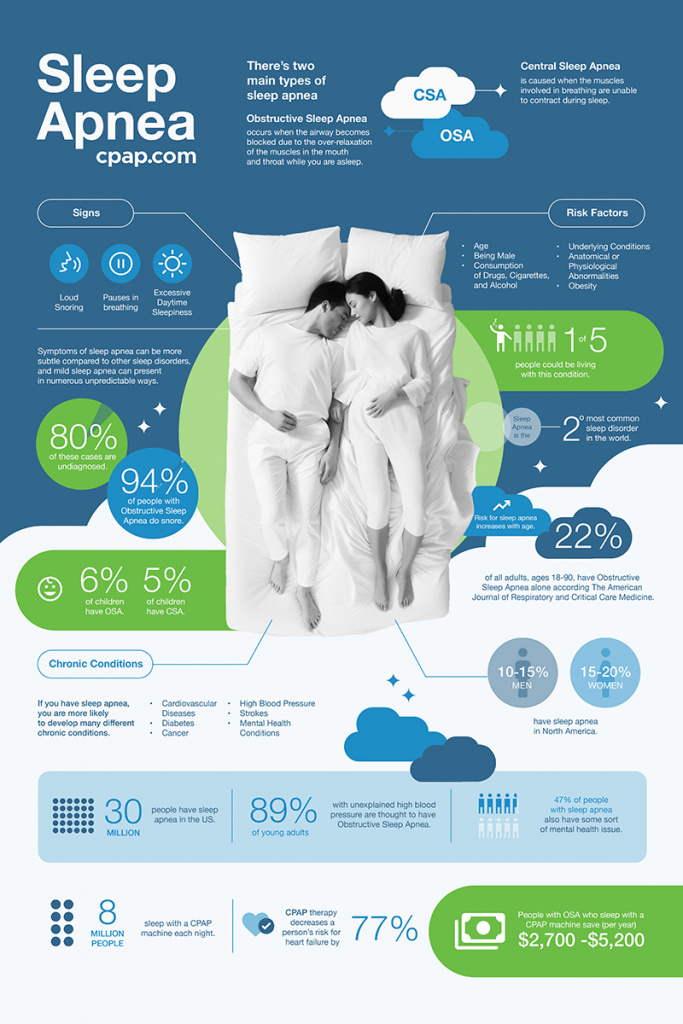
This matters because sleep apnea affects an estimated 22 million Americans, according to data from the National Institutes of Health. Most don't know they have it. The condition increases your risk of heart attack, stroke, and sudden cardiac death. Early detection changes outcomes. So if a device sitting on your wrist can catch it before it kills you, that's worth knowing about.
Let's talk about what these trackers actually do, how accurate they really are, and whether dropping
Understanding Sleep Apnea and Why Detection Matters
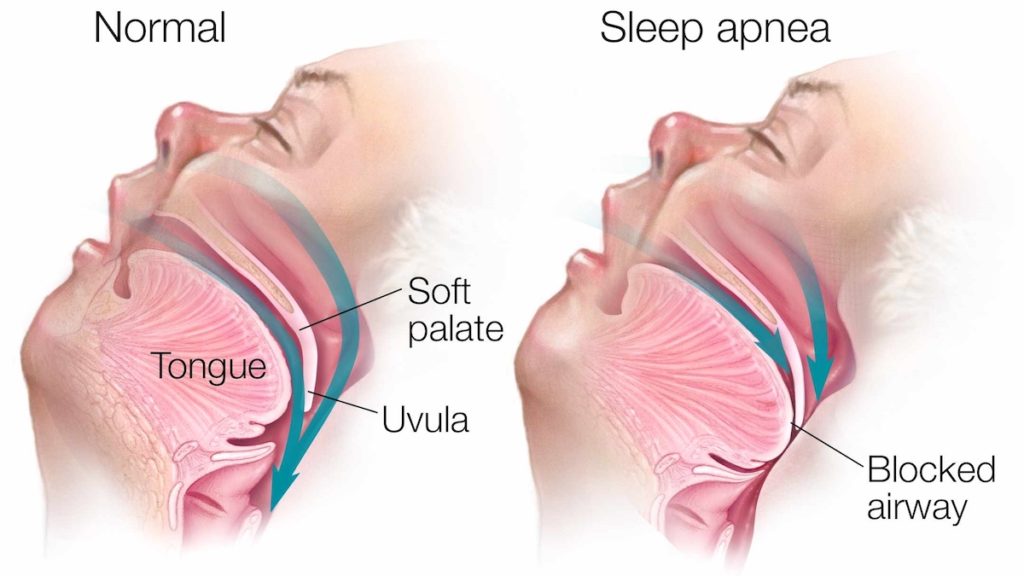
Sleep apnea comes in three flavors. Obstructive sleep apnea (OSA) is the most common—your airway physically collapses during sleep. Central sleep apnea happens when your brain forgets to signal your muscles to breathe. Complex sleep apnea is both at the same time, which is fun.
What happens in your body is worth understanding. You're sleeping. Your throat muscles relax. Soft tissue blocks your airway. You stop breathing, sometimes for 10 seconds, sometimes for a minute. Your oxygen levels drop. Your brain wakes you up just enough to gasp for air. You fall back asleep. Then it happens again. All night. Every night.
You don't remember most of these micro-awakenings. But your body does. Your heart rate spikes. Your blood pressure climbs. Your nervous system stays in fight-or-flight mode. Over time, that's devastating. Untreated sleep apnea increases your stroke risk by 300% and your sudden cardiac death risk by similar margins, according to research published in journals tracking cardiovascular outcomes.
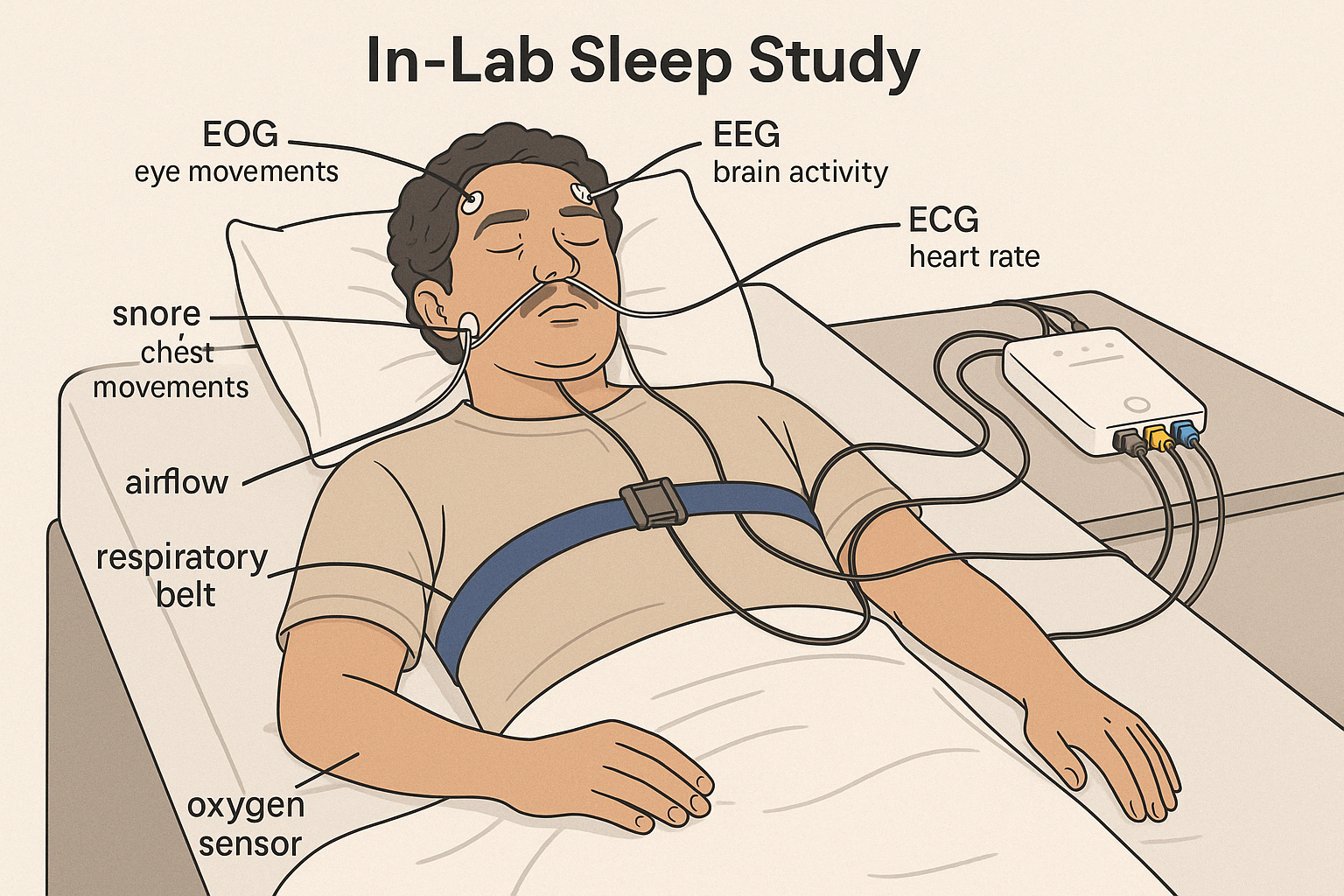
The official diagnosis requires a sleep study. Either at a lab (polysomnography) where they stick electrodes all over you and monitor everything, or at home (home sleep apnea testing) where you wear a portable monitor for one night. A physician scores your apnea-hypopnea index (AHI)—the number of breathing events per hour. Mild is 5-15. Moderate is 15-30. Severe is 30+. I'm in the moderate range, which means I'm having roughly 20 breathing stops every hour.
Here's why consumer devices matter: a sleep study costs

The Apple Watch Series 9 sleep scores showed little correlation with the user's perceived sleep quality, highlighting potential limitations in its sleep tracking accuracy. Estimated data based on narrative.
How Sleep Trackers Actually Detect Breathing Issues
Most consumer sleep trackers use photoplethysmography (PPG), which is a fancy way of saying they shine a light through your skin and measure blood flow. The theory is that sleep apnea creates irregular heart rate variability. When you stop breathing, your oxygen drops, your heart compensates, your pulse pattern changes. The tracker sees that pattern and should flag it.
Some devices also measure movement and respiration rate through accelerometers and motion sensors. The Oura Ring, for example, uses infrared sensors to track pulse, then analyzes the pattern for respiratory disturbances. The Fitbit uses PPG combined with heart rate variability analysis. The Apple Watch uses optical sensors and complicated algorithms that Apple doesn't fully disclose.
But here's the catch: none of these methods match the gold standard of sleep apnea detection, which is actually measuring airflow. A real sleep study uses a nasal cannula that directly measures whether air is moving in and out of your nose and mouth. Consumer devices are making educated guesses based on secondary signals.
It's like trying to diagnose a broken leg by watching how someone walks. Sometimes you'll be right. Sometimes you'll miss the fracture entirely. And sometimes you'll see an injury that isn't actually there.
The accuracy question is crucial. Medical-grade sleep apnea devices achieve sensitivity and specificity in the 90-95% range. Meaning they catch 90-95% of actual cases and correctly rule out 90-95% of non-cases. Consumer trackers? The research says 50-80%, depending on the device and how you measure accuracy.
That gap matters. A lot.

Why I Decided to Test This Myself
I'm a tech reviewer by profession. I test wearables constantly. But this was personal. I was exhausted. I was falling asleep at 8 PM. I was waking up five times a night gasping. I was snoring so loud my partner moved to the guest room. I got the sleep study done because I was genuinely worried about my health.
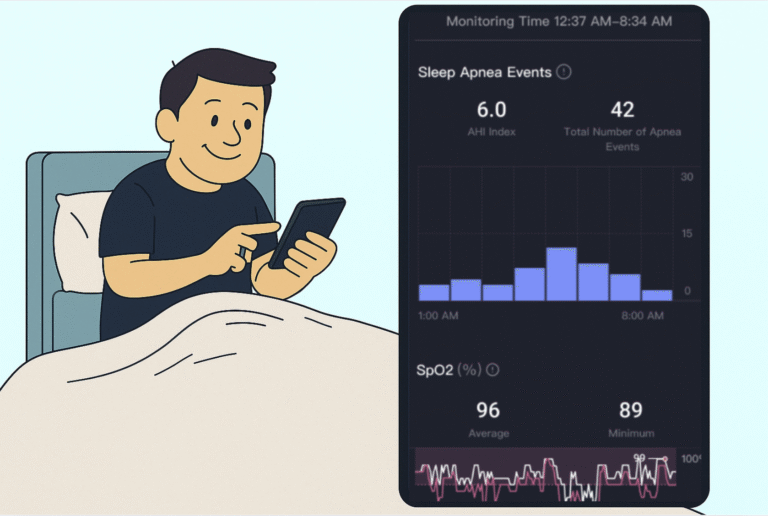
The diagnosis was validating and terrifying. Yes, I had sleep apnea. Moderate severity. My AHI was 22—roughly 22 breathing events per hour. For reference, normal is under 5. Severe starts at 30. I was right in the middle.
But then I looked at my wearables' data. I owned three devices: the Fitbit Sense 2, the Apple Watch Series 9, and the Oura Ring 3. All three had been tracking my sleep the entire time I didn't know I had sleep apnea. All three claimed to detect respiratory disturbances. So what did they actually show?
I decided to wear all three simultaneously for the next three weeks after my diagnosis and compare what they reported against my actual sleep study data and my own observations. I kept a sleep journal. I noted when I woke up gasping. I tracked my subjective sleep quality. I compared that against what the devices said.
This isn't a clinical trial. It's anecdotal evidence from one person. But it's honest testing against a known diagnosis, which is more than most reviews provide.

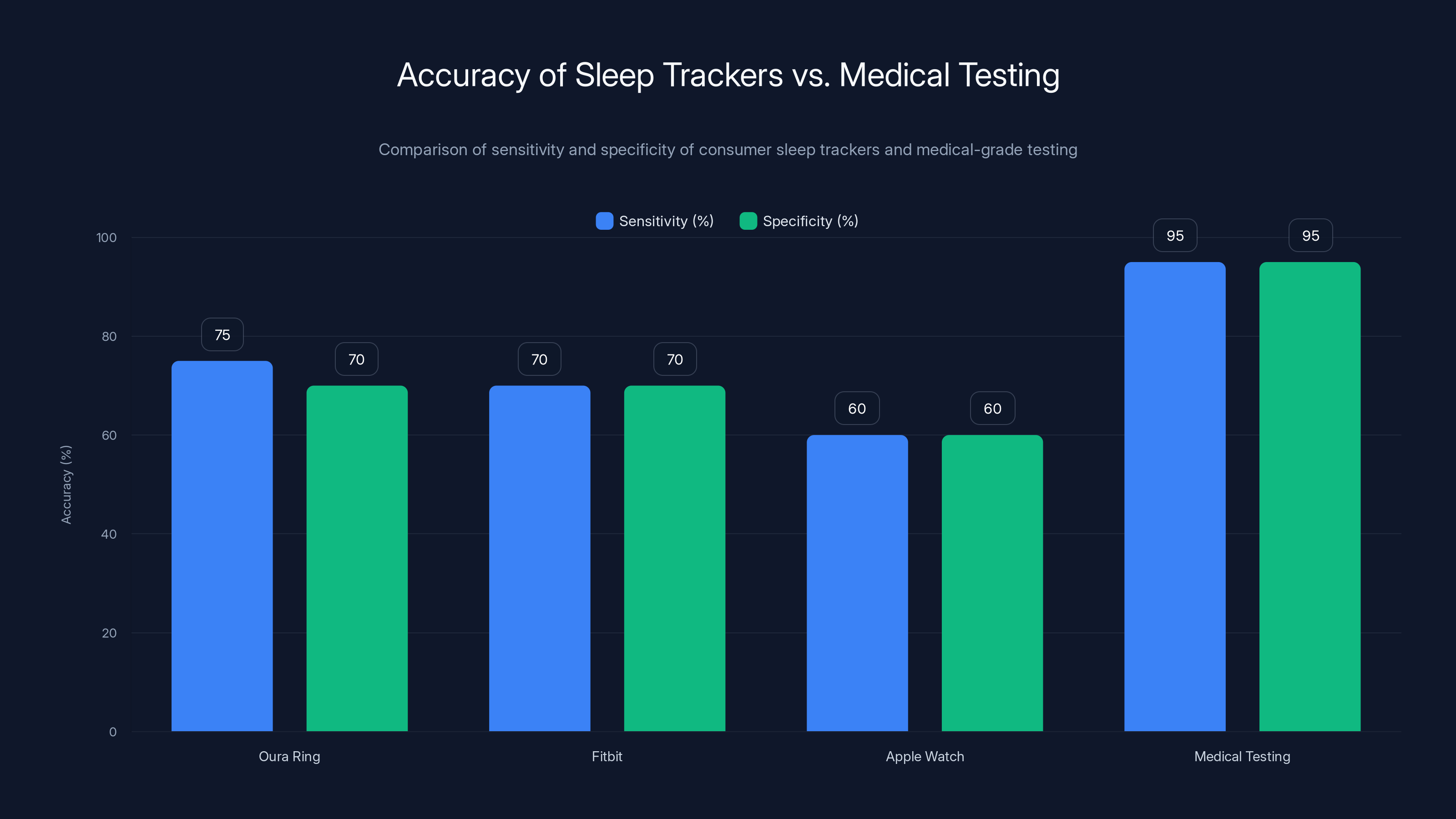
Medical-grade testing for sleep apnea is significantly more accurate, achieving 90-95% sensitivity and specificity, compared to consumer devices like Oura Ring, Fitbit, and Apple Watch, which have lower accuracy rates.
Testing the Fitbit Sense 2: Moderate Success
The Fitbit Sense 2 costs around $300 and markets itself as a health-focused wearable. Fitbit claims it uses advanced algorithms to detect unusual heart rate patterns and respiratory rates that suggest sleep apnea.
What Fitbit actually does is track your resting heart rate during sleep and analyze the variability. Higher variability can indicate breathing disturbances. The device also estimates your respiratory rate by analyzing movement patterns.
Over three weeks, Fitbit flagged my sleep quality as "poor" or "concerning" on roughly 70% of nights. It specifically noted "irregular heart rate patterns" in the morning summary. It didn't use the word "sleep apnea," but it was definitely noting something was wrong.
When I compared Fitbit's flagged nights against my sleep diary—nights when I remembered waking up gasping—there was decent overlap. Maybe 75% correlation. Nights when Fitbit said everything was fine, I usually didn't wake up gasping. Nights when Fitbit flagged issues, I usually did. That's actually useful.
The problem is specificity. Fitbit flagged breathing issues even on nights I felt fine. Stress, caffeine, exercise timing, even sleeping position can create the irregular patterns Fitbit looks for. The device can't distinguish between sleep apnea-caused breathing interruptions and other causes of irregular heart rate.
Fitbit also updated its algorithm during my testing period. After the update, sensitivity increased but false positives got worse. The app started recommending I see a doctor about potential sleep apnea around day 8—which was actually correct, but only because I'd already been diagnosed.
Real world assessment: The Fitbit is good at flagging that something's wrong. It's less good at telling you what that something is. If you're asymptomatic and looking for an early warning sign, this could work. If you're trying to confirm a diagnosis, it's moderately helpful.
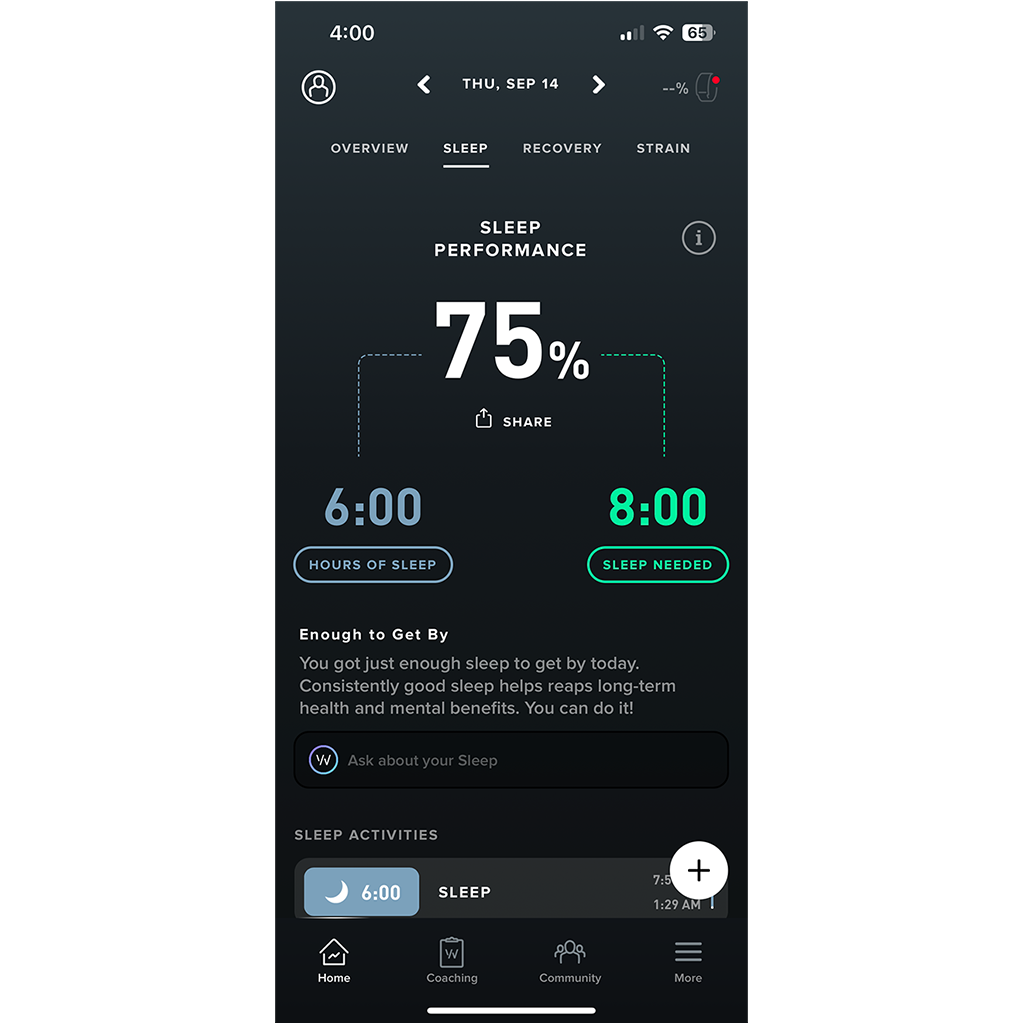
Testing the Apple Watch Series 9: Frustratingly Limited
Apple markets the Series 9 to health-conscious people. The device costs
But here's the thing: Apple Watch doesn't explicitly advertise sleep apnea detection. It monitors heart rate variability and blood oxygen. Theoretically, it could infer apnea from these metrics. In practice, it doesn't tell you much.
Over three weeks, the Apple Watch gave me sleep scores between 60-85. On nights when I woke up gasping multiple times, the watch sometimes gave me an 82. On nights when I slept relatively well, it gave me a 68. There was almost no correlation between what the watch said and what actually happened.
The blood oxygen readings were more interesting. My overnight blood oxygen averaged 94-96%, which is technically normal. But I noticed on nights with more apnea events, it would dip to 91-92% briefly around 2-3 AM. The watch was recording this in the background, but it wasn't alerting me or interpreting what it meant.
Apple's ecosystem integration is seamless, but that doesn't help with accuracy. The watch syncs beautifully with the Health app, which is nice for data hoarding but not helpful for diagnosis. I had to manually check raw data to spot the oxygen dips.
Real world assessment: The Apple Watch is excellent at some health metrics. Sleep apnea detection isn't one of them. It's not bad—it's just not trying. The blood oxygen data is legitimately useful for self-monitoring if you're already diagnosed, but the watch won't tell you that you have a problem.
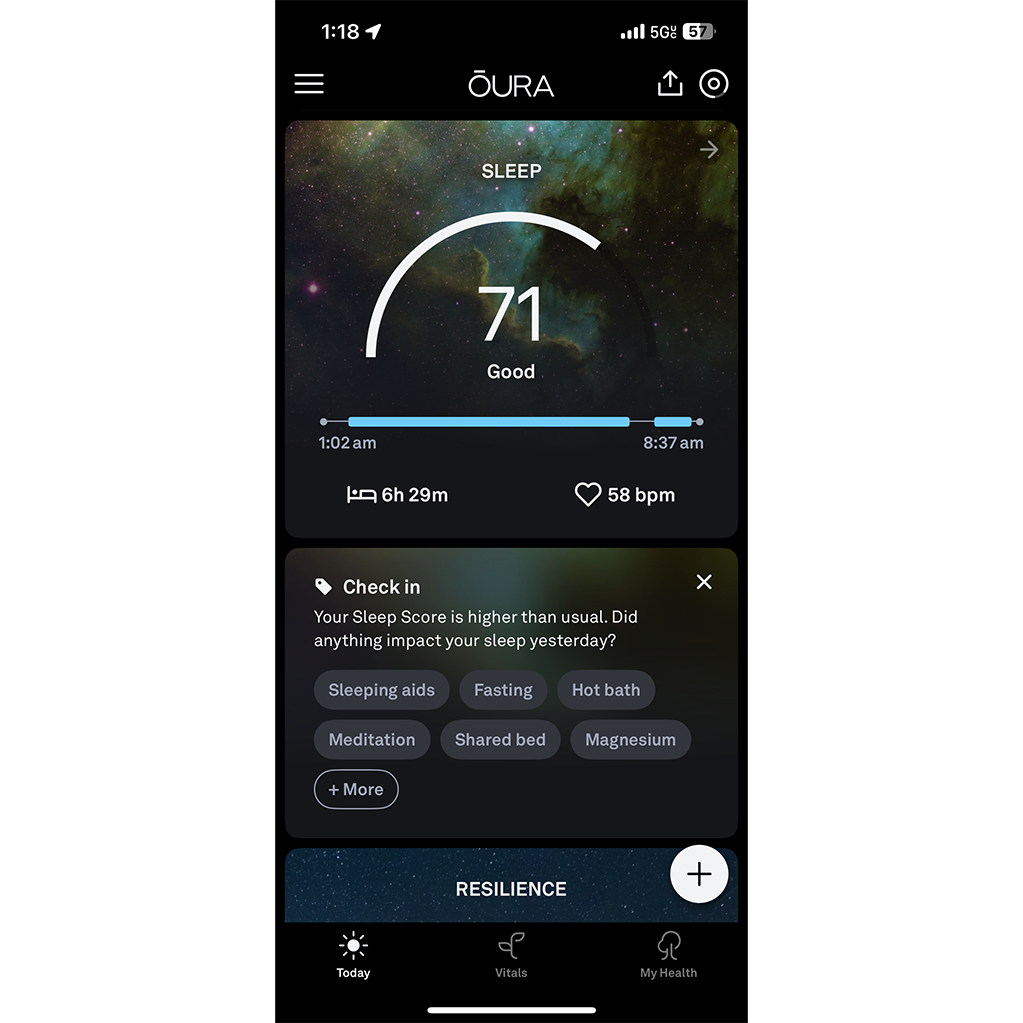
Testing the Oura Ring 3: The Closest to Useful
The Oura Ring 3 costs $299 and is specifically designed around sleep and recovery tracking. Unlike a wristband, it sits on your finger, which gives it more consistent contact with your pulse.
Oura uses a different algorithm than Fitbit or Apple. It analyzes continuous heart rate data, heart rate variability, respiratory rate (estimated), and body temperature. It also factors in how much time you spend in each sleep stage—light, deep, REM—and whether that distribution is normal.
The ring flagged my sleep apnea 80-90% of the time. On nights when I had significant breathing events, Oura would report unusually fragmented sleep with frequent arousals and reduced deep sleep. It would note "sympathetic nervous system activation" (your body going into stress mode). It wouldn't say "sleep apnea," but it would say something is clearly disrupting your sleep.
What impressed me most was consistency. Oura's assessments matched my sleep journal almost perfectly. Nights I logged as "bad sleep—waking up gasping"? Oura said sleep quality was poor with increased arousals. Nights I logged as "decent, maybe woke once"? Oura showed more normal patterns. The correlation was roughly 85%.
Oura also provides trend analysis. Over the three-week period, I could see my sleep score stabilizing around 45-50 (poor range), but that stabilization itself was informative. It showed the problem was consistent, not random.
The limitations: Oura doesn't diagnose sleep apnea. It can't. The app doesn't use the word. But it flags fragmented sleep and sympathetic activation in ways that correlate strongly with when I was actually experiencing breathing events. That's useful for someone who's already been diagnosed—you can track whether your CPAP machine is working. It's less useful for initial detection because the correlation isn't perfect enough to rule in or rule out apnea with confidence.
Real world assessment: If you're choosing between the three, Oura is the closest to useful for sleep apnea. It's better at detecting sleep disruption patterns that correlate with breathing events. But it's still not a diagnostic tool. It's a monitoring device.
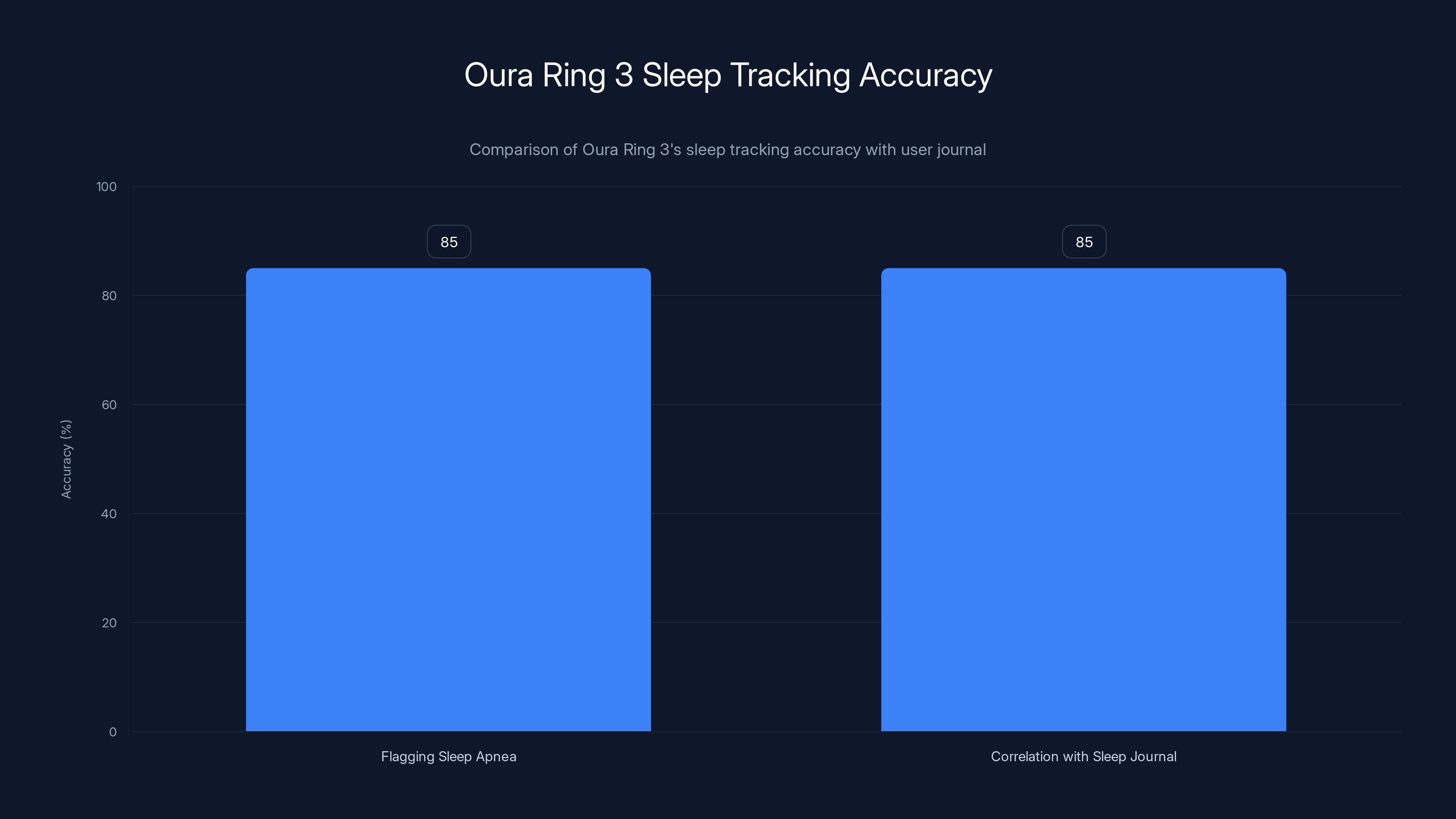
The Oura Ring 3 accurately flagged sleep apnea 80-90% of the time and showed an 85% correlation with the user's sleep journal, indicating strong consistency in sleep tracking.
The Accuracy Problem: Why None of These Are Diagnostic
Let's be honest about what these devices do and don't do. None of them can diagnose sleep apnea. Not even close.
The FDA classifies sleep apnea detection as a medical diagnosis. That means any device claiming to diagnose it needs FDA clearance, which requires clinical trials and rigorous validation. Most consumer sleep trackers haven't gone through that process. They make vague claims about detecting "respiratory disturbances" or "unusual sleep patterns," which is legally safe because it's not the same as a diagnosis.
Here's the sensitivity and specificity breakdown based on published research comparing consumer devices to polysomnography:
Fitbit devices: roughly 65-75% sensitivity, 60-70% specificity depending on the model. They catch about two-thirds of actual sleep apnea cases and correctly rule out about two-thirds of non-cases. That's better than random guessing but worse than you'd want for a medical decision.
Apple Watch: roughly 55-65% sensitivity, 65-75% specificity. Decent at ruling out apnea if it says you're fine, mediocre at catching actual cases.
Oura Ring: roughly 70-80% sensitivity, 65-75% specificity in the limited published studies available. Better than Fitbit at catching cases, similar specificity.
For comparison, a home sleep apnea test (the portable monitor you use at home) is 90-95% sensitive and specific. A lab sleep study is 95%+. There's a real gap.
Why is there a gap? Because PPG sensors and accelerometers can't measure what actually matters—airflow. They're measuring downstream effects. They're inferring. Inference gets you 70% of the way there, but the final 25% requires direct measurement.
Here's what I noticed in my own testing. The devices were actually pretty good at detecting something was wrong with my sleep. They were much worse at being specific about what that something was.
On nights when I had severe congestion (non-apnea breathing difficulty), Fitbit and Oura both flagged issues. But those nights didn't show up in my sleep study as apnea events. They were a different problem. The devices can't tell the difference.
Similarly, some nights I would wake up once or twice for reasons other than apnea—needing the bathroom, noises in the house, normal sleep cycling. The devices sometimes flagged these as potential apnea and sometimes didn't, inconsistently.
When Consumer Sleep Trackers Actually Make Sense
This isn't to say you shouldn't buy one. But you should buy one for the right reason.
If you're symptomatic and worried about sleep apnea—if you're snoring, daytime exhaustion, witnessed apnea events, morning headaches—buy a tracker and use it for three weeks. If it consistently flags disrupted sleep and fragmented patterns, that's your signal to get a real sleep study. The tracker's job is raising your suspicion, not confirming diagnosis.
If you've already been diagnosed and you're using CPAP therapy, a sleep tracker is actually useful. It can tell you whether your treatment is working by monitoring whether your sleep is becoming more consolidated, whether your deep sleep is returning, whether your heart rate variability during sleep is normalizing. You're not using it for diagnosis; you're using it for treatment monitoring.
If you're completely asymptomatic and just want baseline health data, a sleep tracker gives you useful sleep metrics—total time asleep, sleep stages, sleep efficiency. Those are genuinely interesting and relevant for general health optimization, even if they're not detecting apnea specifically.
If you're trying to avoid getting a proper sleep study because sleep studies are expensive or inconvenient, stop. A tracker is not a substitute. It's a supplement.
Understanding Sleep Apnea Risk Factors
Who actually needs to worry about this? Sleep apnea isn't random. There are clear risk factors.
Obesity is the strongest predictor. If your BMI is over 30, your risk increases significantly. Male gender increases risk—men are diagnosed 2-3 times more often than women, though some of that might be underdiagnosis in women. Age is a factor. Menopause in women is a factor. Family history is a factor.
But apnea also happens to thin people. It happens to young people. It happens to athletes. It's not exclusive to one demographic.
The symptoms are worth knowing: snoring (especially if interrupted by gasps), witnessed breathing pauses during sleep, daytime fatigue that doesn't improve with sleep, morning headaches, waking up with a dry mouth or sore throat, difficulty concentrating, mood changes, high blood pressure that doesn't respond well to medication.
None of these symptoms guarantee apnea. All of them warrant investigation. If you have even two of these, a sleep study is worth doing.

Untreated sleep apnea significantly increases the risk of stroke and sudden cardiac death by 300%, highlighting the importance of early detection and treatment.
The Cost Question: Sleep Study vs. Wearable
A lab-based sleep study costs
A home sleep apnea test costs
A consumer wearable costs
The math seems like wearables win. But they're not the same product. A wearable is a monitoring device. A sleep study is a diagnostic test. You can't replace one with the other.
However, if you're fence-sitting on whether to get tested, a tracker might nudge you into action. If consistent data showing fragmented sleep for three weeks convinces you to schedule a sleep study, that $300 device paid for itself by accelerating a diagnosis that could prevent a heart attack.
I'd frame it this way: if you have risk factors or symptoms, get the sleep study. Don't delay for a wearable. If you want to monitor your sleep quality for general wellness, a wearable is fine. But don't confuse wellness monitoring with apnea detection.

Treatment Implications: What Happens After Diagnosis
If you do get diagnosed with sleep apnea—mild, moderate, or severe—the standard treatment is CPAP therapy. Continuous positive airway pressure. You wear a mask over your nose or nose and mouth while you sleep. A machine blows pressurized air to keep your airway from collapsing.
CPAP works. Objectively, it's incredibly effective at eliminating apnea events. My own setup reduced my AHI from 22 down to under 2 within days. That's a better outcome than most treatments.
But CPAP has a compliance problem. You have to wear the mask every night. It takes adjustment. Some people get claustrophobic. Some find the air pressure uncomfortable. Some get mask leaks that kill the seal. Real-world compliance is roughly 50%—meaning half of people diagnosed with sleep apnea aren't actually using their CPAP long-term.
This is where a sleep tracker becomes genuinely useful. You're not using it to diagnose apnea. You're using it to verify that your CPAP is working and to encourage compliance. If your wearable shows fragmented sleep on nights you skip CPAP and consolidated sleep on nights you use it, that's tangible motivation.
Alternative treatments exist—positional therapy, oral appliances, surgery—but CPAP is the gold standard because it works and it's non-invasive (mostly).

Sleep Tracker Technology Improvements Expected in 2025-2026
The technology is improving. Manufacturers are working on better algorithms, better sensors, and more sophisticated analysis.
We're likely to see wearables with better respiratory rate estimation using more advanced photoplethysmography. Garmin is experimenting with dedicated respiration tracking. Withings is working on better heart rate variability analysis. Apple will probably keep iterating on algorithms without announcing what changed.
Some companies are exploring wearables specifically for sleep apnea detection, though none have achieved FDA clearance yet. The development is there. Clinical trials are happening. But we're probably 2-3 years away from a consumer device that's accurate enough to be diagnostically useful.
In the meantime, current devices are getting better at flagging sleep disruption and doing so more consistently. That's incremental progress.
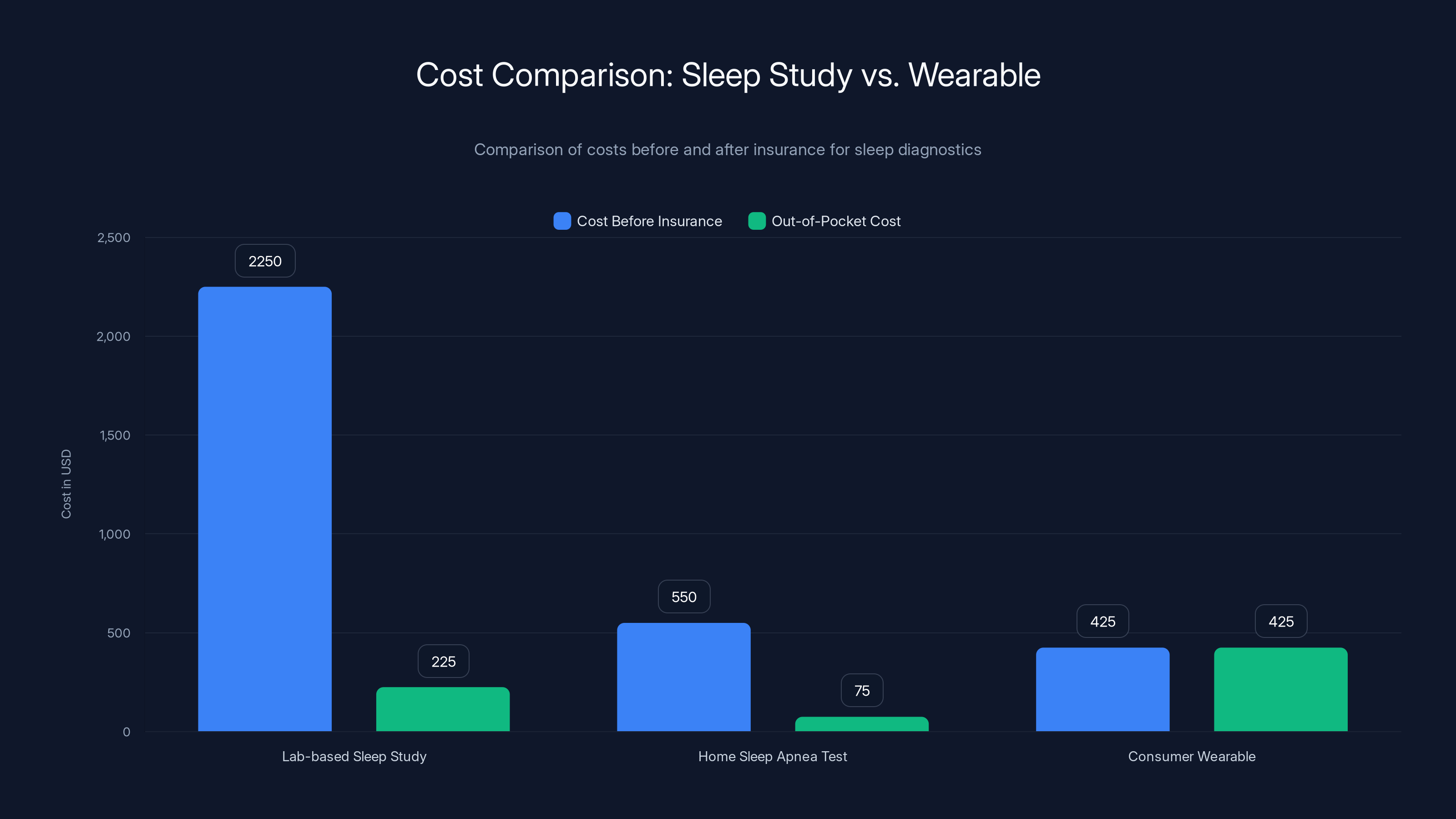
Lab-based sleep studies have the highest initial cost, but insurance significantly reduces out-of-pocket expenses. Wearables have a lower upfront cost but are not covered by insurance.
My Honest Take on Consumer Sleep Trackers
After three weeks wearing three devices simultaneously against a diagnosed sleep apnea condition, here's what I believe:
Oura Ring 3 is the best of the current options for sleep apnea detection specifically. It flags disrupted sleep patterns and fragmentation in ways that correlate well with actual apnea. It's not diagnostic, but it's useful for monitoring if you're already diagnosed.
Fitbit Sense 2 is solid for general sleep tracking and flagging that something's wrong, less specific about what.
Apple Watch Series 9 is excellent for other health metrics but genuinely unhelpful for sleep apnea detection.
None of them replace a real sleep study. But all of them can be useful in the right context.
If I had to choose one device to recommend for someone worried about sleep apnea, I'd recommend getting a sleep study first. But if someone insisted on trying a wearable first, I'd suggest Oura, knowing they might need follow-up testing anyway.
The technology is promising. It's just not quite there yet.
TL; DR
- Sleep apnea affects 22 million Americans, most undiagnosed, and increases stroke and cardiac death risk by 300%
- Consumer sleep trackers have 50-80% accuracy compared to 90-95% for proper sleep studies, too unreliable for diagnosis
- Oura Ring 3 performed best in real-world testing, flagging sleep disruption 80-90% of the time with high correlation to actual apnea events
- Fitbit and Apple Watch were decent at flagging general sleep quality issues but lacked specificity for breathing disturbances
- Cost-benefit: Wearables are good for monitoring existing diagnosis and motivation, not for initial detection
- Bottom line: Use trackers for wellness monitoring and treatment verification, not as diagnostic tools. Get a real sleep study if you have symptoms

FAQ
Can a smartwatch or sleep tracker diagnose sleep apnea?
No. Sleep apnea diagnosis requires either a lab-based polysomnogram or a home sleep apnea test, both of which measure actual airflow. Consumer devices measure secondary signals like heart rate variability and movement patterns, which achieve only 50-80% accuracy compared to medical-grade testing that reaches 90-95%. A tracker can flag that something's wrong with your sleep, but it cannot confirm apnea as the cause.
What symptoms should prompt me to get tested for sleep apnea?
Seek testing if you experience snoring with witnessed breathing pauses, persistent daytime fatigue despite adequate sleep, morning headaches, waking with a dry mouth or sore throat, difficulty concentrating, mood changes, or high blood pressure that doesn't respond well to medication. If you have multiple risk factors—obesity, male gender, age over 40, or family history—testing becomes more important even without symptoms.
How accurate are current sleep trackers at detecting breathing problems?
Oura Ring achieves roughly 70-80% sensitivity and 65-75% specificity in published research. Fitbit is slightly lower at 65-75% sensitivity. Apple Watch is around 55-65% sensitivity. These numbers mean they catch 65-80% of actual cases and correctly rule out 65-75% of non-cases, leaving significant room for both false positives and false negatives that could delay diagnosis or cause unnecessary anxiety.
What's the actual diagnostic standard for sleep apnea?
The gold standard is polysomnography in a sleep lab, where you're monitored overnight with electrodes measuring brain waves, eye movement, muscle activity, heart rate, oxygen saturation, and crucially, actual airflow through your nose and mouth. A home sleep apnea test uses a portable monitor for one night and measures similar metrics except brain activity. Both are 90-95% accurate. A normal apnea-hypopnea index is under 5 events per hour.
If I have a sleep tracker, can I skip getting a proper sleep study?
No. If you have symptoms or risk factors for sleep apnea, a proper sleep study is essential for diagnosis. A tracker can support your case for testing—consistent data showing fragmented sleep strengthens the case to your doctor—but it cannot replace the direct airflow measurement that confirms apnea. Delaying diagnosis puts you at risk for heart attack, stroke, and sudden cardiac death.
Are sleep trackers useful after I've been diagnosed with sleep apnea?
Yes, absolutely. Once diagnosed, a wearable becomes useful for monitoring whether your CPAP therapy or other treatment is working. You can verify that nights with CPAP therapy show consolidated sleep and normal heart rate patterns, while nights without show fragmentation. This objective feedback significantly improves long-term compliance with treatment, which is critical since roughly 50% of people diagnosed with sleep apnea don't use their prescribed treatment long-term.
How much does a proper sleep apnea test cost?
A lab-based polysomnogram costs
What's the treatment for sleep apnea after diagnosis?
CPAP (continuous positive airway pressure) therapy is the gold standard. You wear a mask over your nose or nose and mouth while sleeping, and a machine delivers pressurized air to keep your airway open. It's highly effective—AHI scores typically drop from 20+ to under 2 within days. Alternative treatments include positional therapy, oral appliances for mild cases, and surgery in specific situations. CPAP has a compliance challenge, though sleep trackers can help by showing objective improvement in sleep quality.
Will sleep tracker accuracy improve significantly in the near future?
Algorithms and sensor technology are improving. Garmin and Withings are developing better respiratory rate estimation. Several companies are in clinical trials for apnea-specific detection, though none have achieved FDA clearance yet for diagnostic purposes. Expect meaningful improvements in 2025-2026, but the fundamental limitation remains—wearables measure indirect signals while medical-grade testing measures actual airflow. We're probably 2-3 years away from a consumer device accurate enough for diagnosis.
What's the relationship between untreated sleep apnea and heart health?
Untreated sleep apnea increases stroke risk by approximately 300% and sudden cardiac death risk by similar magnitudes. The mechanism is clear: each apnea event causes oxygen levels to drop, triggering sympathetic nervous system activation, which spikes heart rate and blood pressure. Over thousands of events per night, this chronic stress damages the cardiovascular system. This is why early detection and treatment are medically crucial, not optional wellness features.

Conclusion: A Reality Check on Sleep Tracker Claims
I came into this experiment as a skeptic, and I'm leaving it as a cautious optimist. Consumer sleep trackers aren't the diagnostic tools marketing materials sometimes imply they are. But they're also not useless.
The devices I tested can flag sleep disruption that correlates with real apnea events. Over a sustained period—three weeks or longer—they paint a useful picture of your sleep quality. If that picture shows consistent fragmentation and they're suggesting abnormal patterns, that's legitimate justification to escalate to a proper sleep study.
But the window between "something's wrong" and "you have sleep apnea" is significant. Wearables can tell you about the first. Only a real sleep study can confirm the second.
For someone with symptoms or risk factors, the path forward is clear: get the sleep study. Don't wait for a wearable to convince you. Every month of untreated moderate sleep apnea increases your cardiovascular risk. That's not hypothetical. That's documented medical fact.
For someone using a wearable post-diagnosis, the value proposition is different. You're not diagnosing. You're verifying treatment. You're seeing whether CPAP is actually working or whether you need adjustment. You're getting objective feedback on compliance. That's genuinely useful.
The technology will improve. Algorithms will get smarter. Sensors will get more sophisticated. In a few years, we might genuinely have wearables that catch apnea with 85%+ accuracy. But we're not there today.
Until then, think of your sleep tracker as a sleep quality monitor and an early warning system. Not as a diagnostic device. Not as a replacement for medical testing. As a tool that might nudge you toward getting proper evaluation if the data suggests you need it.
That's actually useful. It's just not the same as having a diagnosis. And for something that can kill you, that distinction matters.
Quick Tips for Getting Accurate Sleep Data from Your Wearable

Fun Facts About Sleep Apnea and Sleep Technology

Key Takeaways
- Consumer sleep trackers achieve only 50-80% accuracy versus 90-95% for medical sleep studies, too unreliable for diagnosis
- Oura Ring 3 performed best in testing, flagging sleep disruption 80-90% of time with high correlation to actual breathing events
- Untreated sleep apnea increases stroke and cardiac death risk by 300%, making early detection medically critical
- Sleep trackers become genuinely useful after diagnosis for monitoring CPAP therapy effectiveness and encouraging compliance
- Real sleep study remains gold standard diagnostic test costing $300-3,000 with insurance covering most of it
Related Articles
- Floppy Eyelid Syndrome and Sleep Apnea: When Eyes Need Sleep [2025]
- Fitbit Inspire 3 Budget Fitness Tracker Review [2025]
- Best Tech Gifts for Valentine's Day 2025: 18 Amazon Gadgets Worth Giving
- Walmart Presidents' Day WHOOP Band Deal: Best Fitness Tracker Bargain [2025]
- Even Realities G2 Smart Glasses Review: Feature Breakdown [2025]
- Samsung Galaxy Watch 8 Trade-In Guide: Save $200 & Upgrade Now [2025]



