Pharma Execs Strike Back: RFK Jr.'s Vaccine Agenda Under Fire [2025]
Last January, something remarkable happened at the J. P. Morgan Healthcare Conference in San Francisco. Executives from the world's largest pharmaceutical companies, who had spent months carefully tiptoeing around the Trump administration, finally snapped. Pfizer's Albert Bourla didn't mince words: "I am very annoyed. I'm very disappointed. I'm seriously frustrated." Moderna's Noubar Afeyan warned of cascading consequences. Merck's Dean Li predicted a three-year collapse in flu vaccination rates.
They weren't reacting to a surprise earnings miss or a failed clinical trial. They were responding to one man's sweeping assault on the cornerstone of modern medicine: the childhood vaccine schedule.
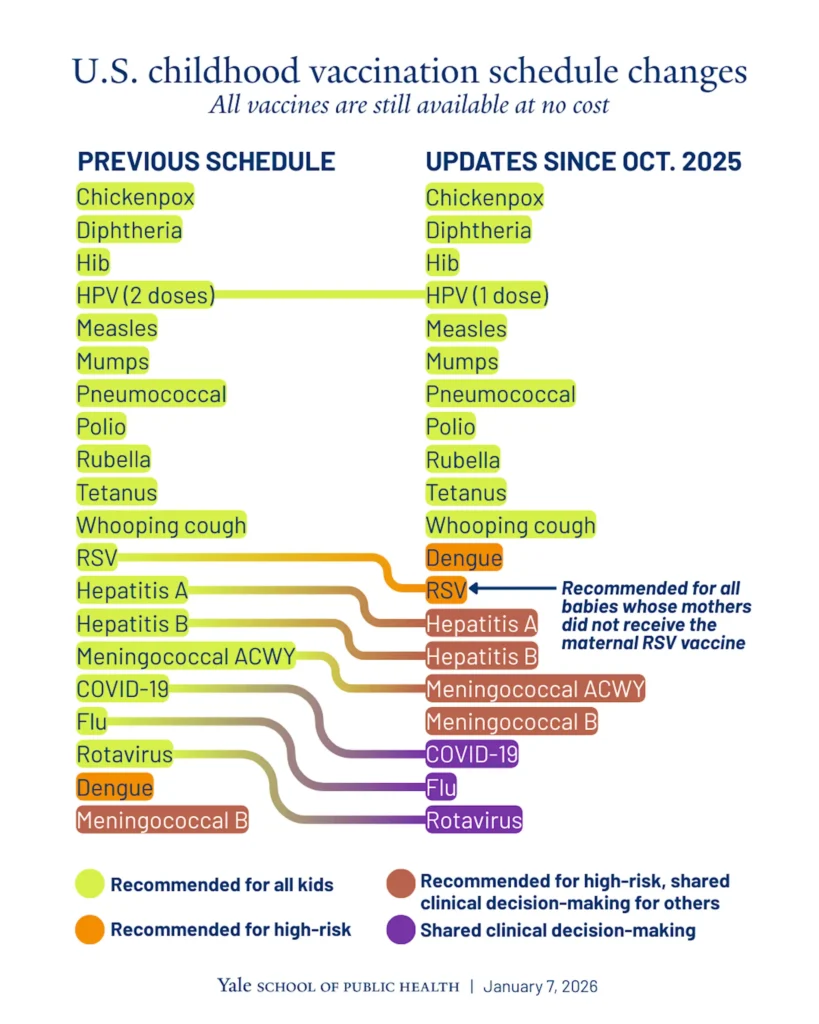
In December 2024, Health Secretary Robert F. Kennedy Jr. and his allies announced a radical overhaul of America's vaccination program, slashing recommended childhood vaccines from 17 to 11—a move that bypassed scientific review, shocked the medical establishment, and triggered what might become the most significant public health battle in a generation. What makes this moment extraordinary isn't just the policy itself. It's that after months of strategic silence, the pharmaceutical industry is finally speaking openly about the existential threat they perceive.
This article digs into the shifting landscape of vaccine policy, why pharma execs abandoned their restraint, what's actually at stake, and what comes next in a conflict that's rapidly reshaping American public health.
TL; DR
- RFK Jr.'s vaccine schedule cuts: Reduced recommended childhood vaccinations from 17 to 11, bypassing normal scientific peer review processes entirely
- Unprecedented pharma pushback: Major executives including Pfizer, Moderna, Merck, and Sanofi CEOs openly criticized the administration's anti-vaccine agenda for the first time
- Broader implications: The move puts the US at odds with peer nations, with only Denmark recommending fewer vaccines; medical groups are preparing legal challenges
- Industry concerns: Pharma leaders worry about litigation risks, declining vaccination rates, and a precedent for attacking other drug categories
- Political calculation: Executives suggest waiting for midterm elections, implying this is a temporary political phenomenon rather than a permanent shift
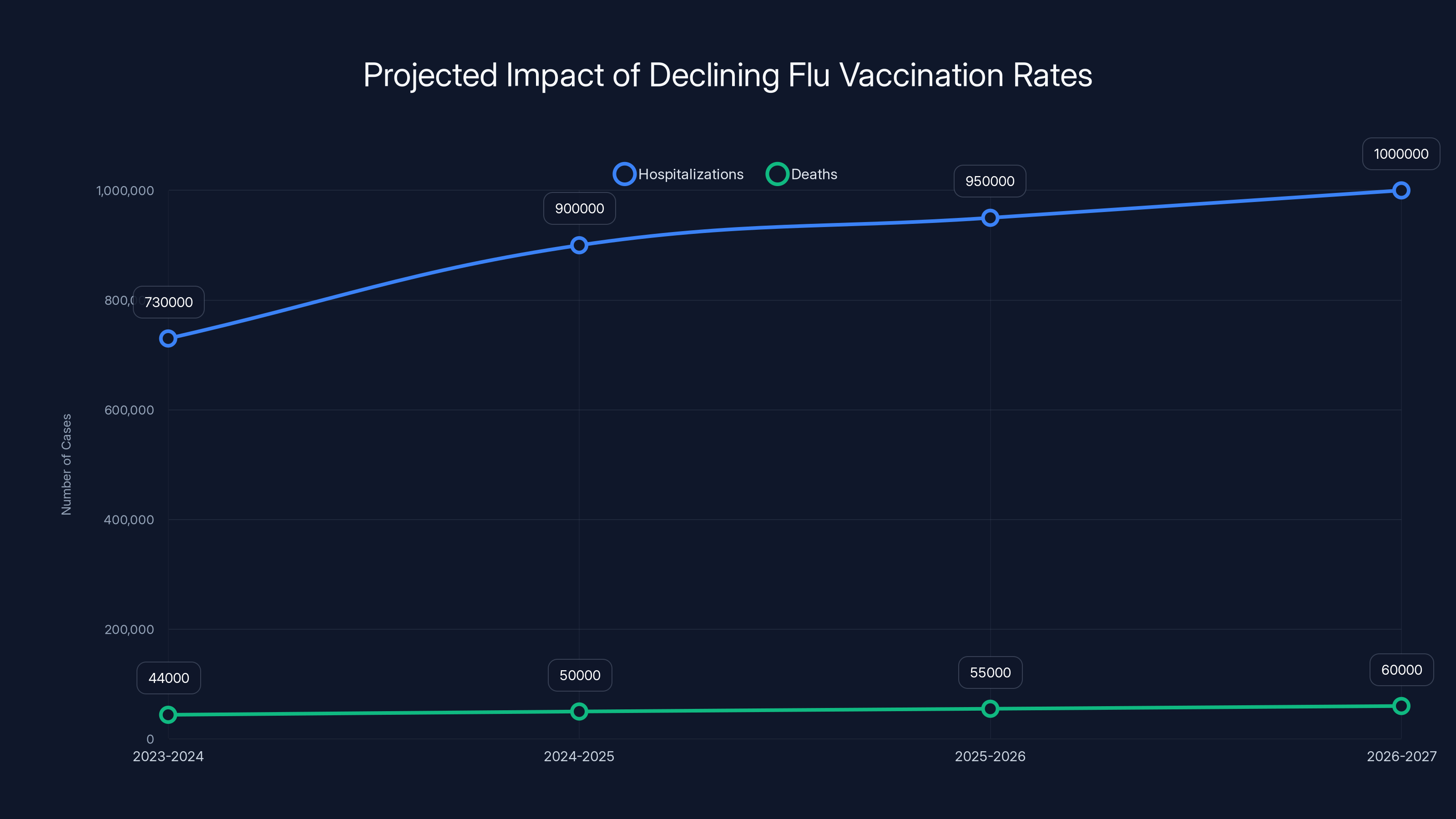
Projected data shows an increase in flu-related hospitalizations and deaths if vaccination rates continue to decline. Estimated data.
Why the Sudden Reversal: Understanding Pharma's Breaking Point
Pharmaceutical executives don't typically burn bridges with sitting administrations. They have too much to lose. Regulatory approval, pricing flexibility, patent protections, and public perception all hang in the balance. For the first year of the Trump administration, major pharma CEOs adopted a posture of quiet negotiation. They hosted meetings, they complied where possible, they hoped that reasonable voices would prevail.
But something changed in December 2024. The vaccine schedule cuts weren't a negotiation or a suggestion. They were a unilateral overhaul announced without prior consultation with the CDC's vaccine advisory committee, without peer-reviewed analysis, without the months-long deliberative process that typically governs such decisions. Kennedy didn't ask for input. He didn't convene scientific experts. He issued the changes as a fait accompli.
That's when the pharmaceutical industry collectively decided that silence was no longer a viable strategy.
"You reach a point where you have to speak up," one Merck executive told reporters at the conference. The calculus had shifted. The reputational risk of staying silent about an attack on vaccines was now greater than the diplomatic risk of speaking out. Bourla's anger wasn't performative. It was the sound of executives realizing that their entire industry—and the scientific credibility of their products—was under threat.
The irony cuts deep. Pfizer and Moderna didn't spend billions developing mRNA vaccine technology to watch it get dismantled by a health secretary who once compared vaccines to thalidomide. Merck didn't invest decades in immunology to be told that childhood vaccination causes autism, a claim that's been thoroughly debunked across multiple massive studies involving millions of children.
For pharma executives accustomed to navigating Washington politics, this felt like a line being crossed. Not just a policy disagreement, but an assault on the scientific method itself.
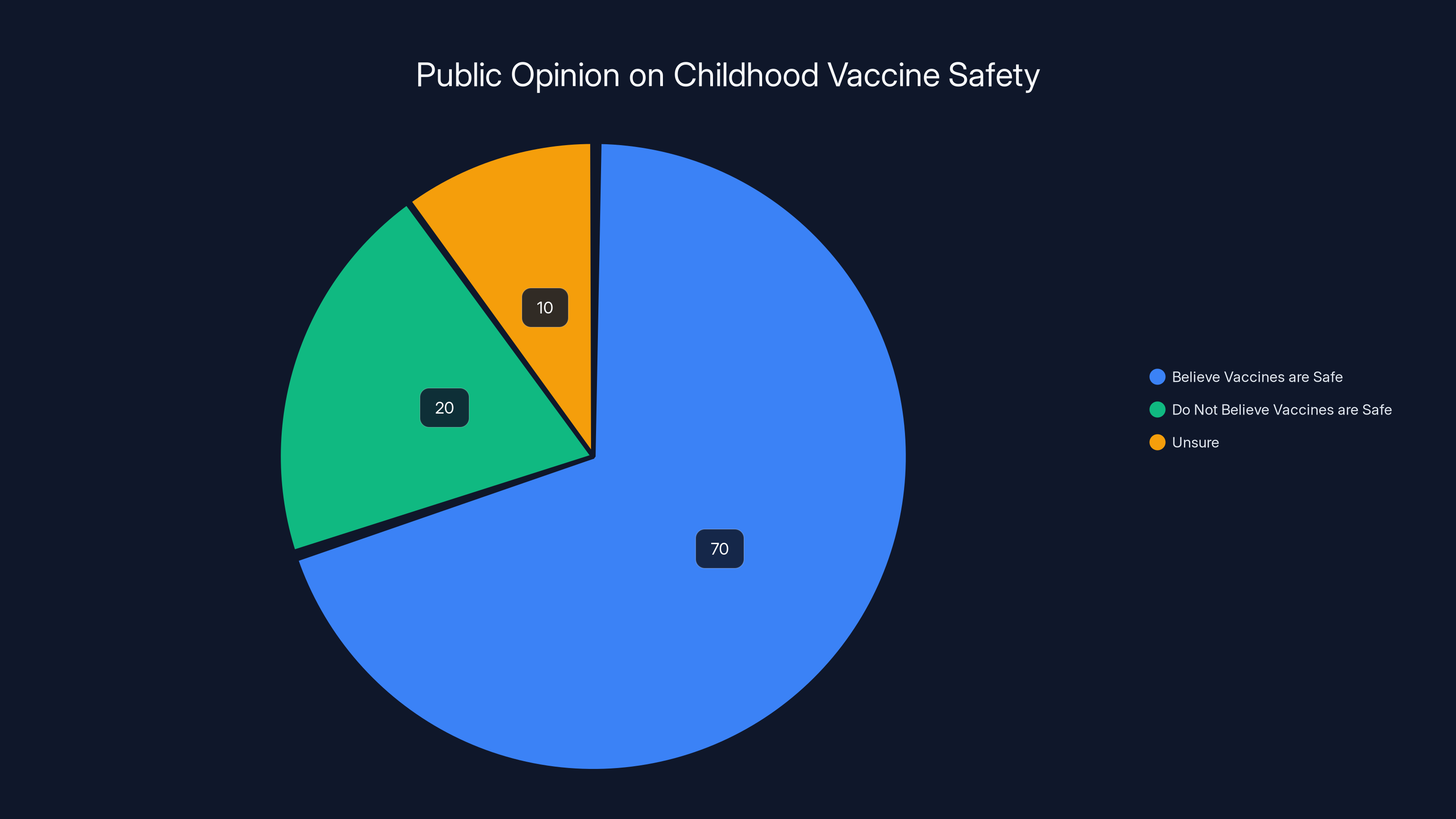
Polling indicates that 70% of Americans believe childhood vaccines are safe, despite anti-vaccine rhetoric. Estimated data based on typical polling results.
The Vaccine Schedule Cuts: What Actually Changed and Why It Matters
Here's what Kennedy did in December 2024: He announced a revised childhood vaccination schedule that cut the number of recommended routine vaccines from 17 to 11. On the surface, that might sound like a minor adjustment—a 35% reduction in the number of shots. But the actual impact is far more severe.
The removed vaccines targeted serious, sometimes fatal diseases. The changes eliminated or delayed protection against:
- Rotavirus (a leading cause of severe diarrhea in infants)
- Hepatitis A (a viral disease that can cause liver failure)
- Several doses of other vaccines moved to later ages
What makes this especially alarming is the process—or rather, the complete lack of one. Normally, any change to the vaccine schedule requires:
- Scientific review by the CDC's Advisory Committee on Immunization Practices (ACIP)
- Peer-reviewed evidence presentation and discussion
- Transparent public meetings where stakeholders can comment
- Documented reasoning and cost-benefit analysis
- Coordination with other health agencies
This process typically takes 6-12 months, sometimes longer. It exists because vaccine recommendations affect hundreds of millions of people over decades. The stakes are enormous. A bad decision could result in disease outbreaks, childhood deaths, and permanent immune system damage.
Kennedy skipped all of it. No ACIP review. No peer-reviewed evidence. No public comment period. No documented reasoning. Just an announcement that the schedule was changing, effective immediately.
"It was the most unscientific decision-making process I've witnessed in 30 years," one pediatrician told colleagues after the announcement. That comment captured the core issue. Pharma wasn't just worried about vaccine sales. They were horrified by the violation of basic scientific process.
The stated justification was that the US would become more "aligned with peer nations." Kennedy claimed that other developed countries use fewer vaccines and achieve better health outcomes. But that claim collapsed under scrutiny.
A rapid analysis by a leading health publication compared vaccine schedules across 20 peer nations. The results were damning for Kennedy's argument. The US, after the cuts, recommends significantly fewer vaccines than almost every comparable country. Australia recommends more. Canada recommends more. Germany, France, Italy, Spain, Sweden, Norway, Japan—all recommend more. Of 20 peer nations examined, only one other country (Denmark) had a similarly sparse vaccine schedule.
In other words, the US didn't become more aligned with international standards. It became an outlier. A negative outlier.
Pfizer's Bourla made this point directly: "The claim that this aligns us with peer nations is false. We've done the research. We've looked at what Germany does, what Canada does, what Australia does. The numbers don't support this narrative." Moderna's Afeyan was blunter: "This isn't science. This is ideology dressed up as policy."
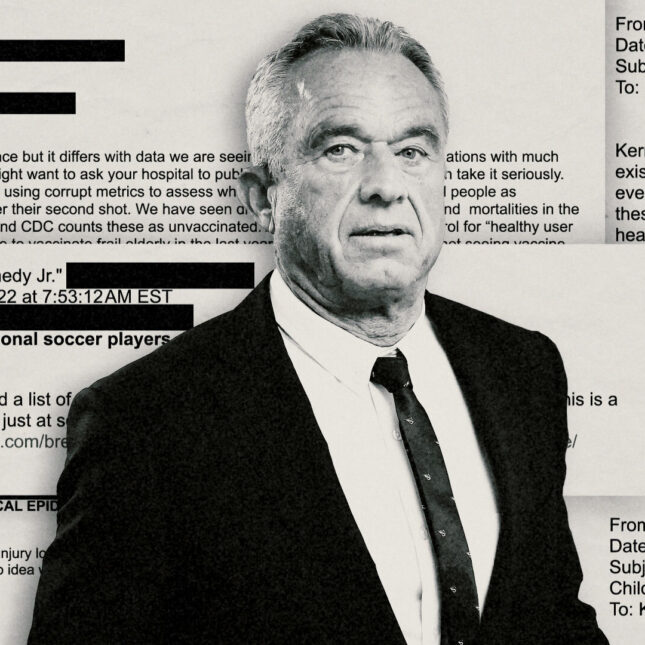
Kennedy's Background: Why Pharma Sees a Threat Beyond Policy
To understand why pharmaceutical executives view Kennedy's leadership with such alarm, you need to understand his background—and his financial incentives.
Robert F. Kennedy Jr. is not a physician. He's not an epidemiologist. He holds no degree in public health, immunology, or medicine. He's an environmental lawyer by training, known for litigation against environmental polluters. That background matters, but his vaccine-related background matters more.
For two decades, Kennedy has been involved in high-profile lawsuits against vaccine manufacturers. He's served as an attorney in cases claiming vaccine injuries. More importantly, he's profited handsomely from these cases. While Kennedy frames himself as an anti-vaccine activist motivated by public health concerns, the financial reality is more complex. His law practice has generated substantial income from vaccine-related litigation.
That's not a casual conflict of interest. It's a structural one. Kennedy's professional success is directly tied to the number and severity of vaccine-injury lawsuits. The more doubt people have about vaccines, the more litigation gets filed. The more litigation, the larger Kennedy's potential paydays.
Pfizer's Bourla highlighted this dynamic explicitly: "There is also a lot of plaintiffs' playbook there. Everybody will start litigating." He wasn't just making an observation. He was pointing out that Kennedy's policy decisions align perfectly with Kennedy's financial interests. Cut the vaccine schedule, generate doubt about vaccines, trigger litigation, and the lawyers—including Kennedy's allies—make money.
Several of Kennedy's key advisors in the Trump administration have similar litigation backgrounds. This isn't a conspiracy theory. It's a documented pattern that pharma executives view as representing a fundamental conflict of interest at the highest levels of health policy.
"We're dealing with people whose financial incentives are directly opposed to public health," one Sanofi executive explained. "That's extraordinarily dangerous in a position of public trust."
For pharma, this context transforms the vaccine schedule cuts from a policy disagreement into something more sinister: a power grab by people with direct financial motivation to undermine confidence in the pharmaceutical industry.
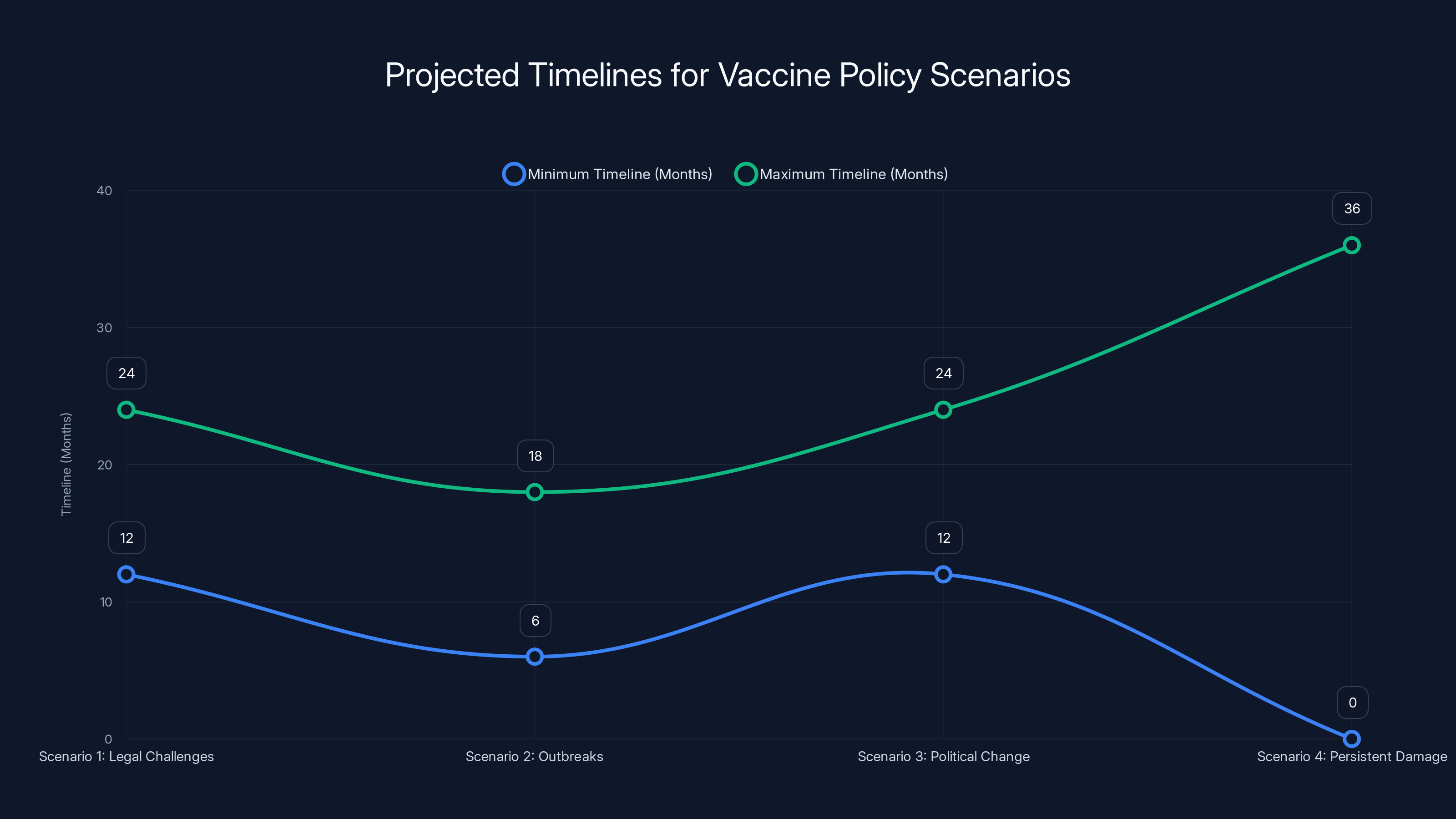
The chart illustrates the estimated timelines for each vaccine policy scenario, highlighting the range of months expected for each outcome. 'Persistent Damage' is ongoing, indicating continuous impact.
The Medical Establishment Fights Back: Legal Challenges and Organized Resistance
The pharmaceutical industry wasn't the first group to push back. The American Academy of Pediatrics (AAP), the nation's primary organization of pediatricians, moved quickly to challenge Kennedy's authority to unilaterally rewrite vaccine policy.
The AAP didn't just criticize the decision. They announced preparation of a formal legal challenge, arguing that Kennedy exceeded his legal authority by bypassing established scientific review processes. The legal theory is straightforward: health secretaries don't have the power to unilaterally rewrite major public health policies without following the administrative procedures established by statute and regulation.
Other major medical organizations followed. The American Medical Association. The Infectious Diseases Society of America. The Immunization Action Coalition. The Public Health Association. This wasn't a fringe response. It was the organized consensus of virtually every credible medical institution in the United States.
Their argument was simple: Kennedy's changes lacked scientific justification, violated established procedures, and put children at risk.
What surprised many observers was the speed and visibility of pharma's alignment with medical groups. Normally, pharmaceutical companies and medical organizations maintain some distance from each other—they disagree on pricing, on marketing, on access. But on the vaccine schedule issue, they moved in lockstep.
This coalition is important because it suggests this isn't a "Big Pharma versus public health" narrative. It's an alliance of doctors, pharmaceutical companies, public health researchers, and medical institutions united around a single question: Should major public health decisions be made through evidence-based scientific processes, or through political ideology?
The legal challenges will likely take months or years to resolve. But the court battles are just one dimension of the resistance. Hospital systems began revising their protocols. Insurance companies started assessing coverage policies. State health departments began requesting clarification from the CDC. The system was actively resisting Kennedy's mandate.
The Flu Vaccination Crisis: What Happens When People Stop Getting Shots
Kennedy's anti-vaccine agenda isn't limited to childhood vaccines. Throughout 2024, anti-vaccine rhetoric intensified around seasonal flu shots. And that terrifies public health officials because flu isn't a trivial disease.
Dean Li, president of Merck Research Laboratories, made a sobering prediction at the healthcare conference: "With the pressure on vaccination, I cannot foresee flu vaccination increasing in this country over the next three years." That's not just a business forecast. It's a warning about a public health crisis.
Consider what happens when flu vaccination rates drop. The 2023-2024 flu season was described as "bad" but not catastrophic by historical standards. About 730,000 hospitalizations and approximately 44,000 deaths. The 2024-2025 season has already tracked worse, approaching 900,000 hospitalizations and potentially 50,000+ deaths.
Now extend that trajectory into a scenario where anti-vaccine sentiment has been amplified by the nation's health secretary. Where social media posts questioning vaccine safety are amplified by influential voices. Where parents who might have gotten their kids a flu shot become uncertain and skip it.
The public health mathematics are brutal. A 10% decline in flu vaccination rates could result in 50,000 additional hospitalizations per year. A 20% decline could mean 100,000 additional hospitalizations. Those aren't abstract numbers. They're individual people experiencing severe respiratory illness, some requiring intensive care, some dying.
Sanofi's Paul Hudson expressed this concern with visible pessimism: "It's clear this administration has a particular sensitivity around vaccination. I'm asked all the time 'what are you going to do to fix this?' The truth is we just need to stay extremely objective and continue presenting the evidence. There's really very little else we can do."
Hudson's resignation about his limited ability to change the course is striking. These are among the most powerful business leaders in the world. They control billions in resources. But when facing a health secretary with an ideological commitment to anti-vaccine policy, they feel relatively powerless.
His suggestion to "wait for the midterm elections" reveals pharma's underlying strategic calculation: they believe this is a temporary political phenomenon that will swing back when voting patterns change. Until then, they're essentially playing defense.

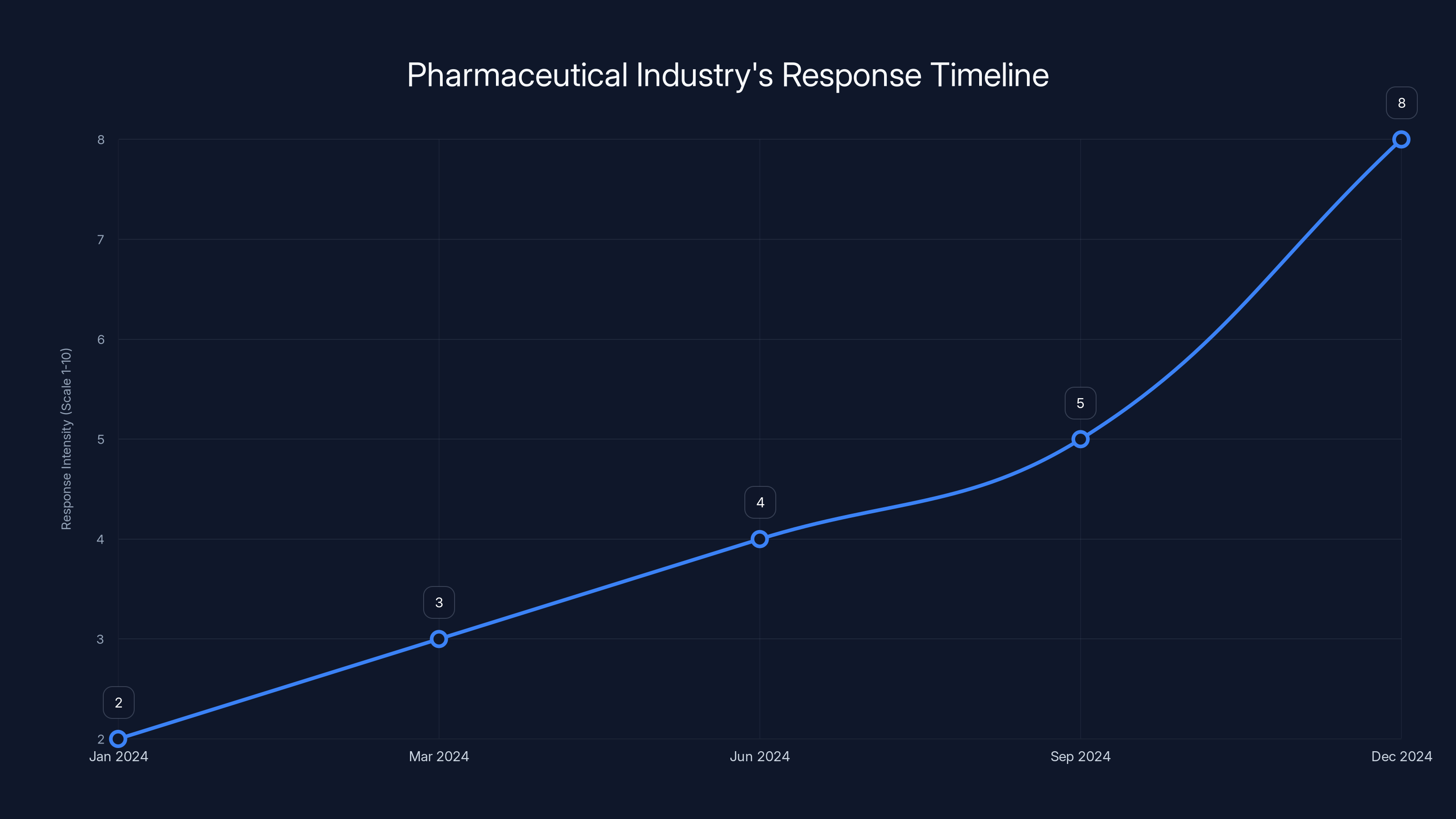
Estimated data shows a significant increase in the pharmaceutical industry's response intensity, peaking in December 2024 due to policy changes.
Defining the Timeline: How Fast Policies Are Being Implemented
One of the most alarming aspects of Kennedy's vaccine initiative is its speed. Within weeks of taking office in January 2025, he had announced the schedule changes. Within months, those changes were rippling through the health system.
Hospitals had to revise their immunization protocols. Pediatricians needed updated guidance. Insurance companies had to adjust coverage decisions. State health departments had to communicate new policies to local providers. The change was disruptive precisely because it was so sudden and because it contradicted established clinical guidelines.
Typically, major policy shifts happen over 12-24 months to allow for proper implementation. Kennedy compressed that into weeks. For someone skeptical of vaccines, this speed is a feature—it prevents the medical establishment from mobilizing opposition. For public health professionals, it's a bug—it prevents proper rollout and creates confusion.
The Litigation Playbook: Why Pharma Fears the Legal Landscape Ahead
Bourla's comment about the "plaintiffs' playbook" deserves deeper examination because it reveals pharma's deepest fear: not just policy changes, but a systematic legal assault on the entire vaccine industry.
Vaccine litigation exists. It has legitimate cases and frivolous ones. Courts have systems to distinguish between them. But what happens when the nation's health secretary is actively promoting vaccine skepticism? When influential voices are claiming vaccines cause autism, that vaccines contain toxins, that the CDC is engaged in a conspiracy?
All of that generates cases. Many will lack merit. But some will proceed through the legal system. And in a polarized environment where a significant portion of the public believes vaccines are dangerous, jury trials become unpredictable. A jury that's been exposed to anti-vaccine messaging might be sympathetic to claims that would be laughed out of court under normal circumstances.
Pharmaceutical companies have deep pockets for litigation. But litigation is expensive. A wave of vaccine cases—even mostly frivolous ones—represents millions in legal fees and years of management attention. And worst case scenario: a jury verdict against a vaccine manufacturer, however scientifically unsound, could have massive implications for the entire industry.
This isn't paranoia. It's a realistic assessment of legal risk in an environment where vaccine skepticism has high-level government support.
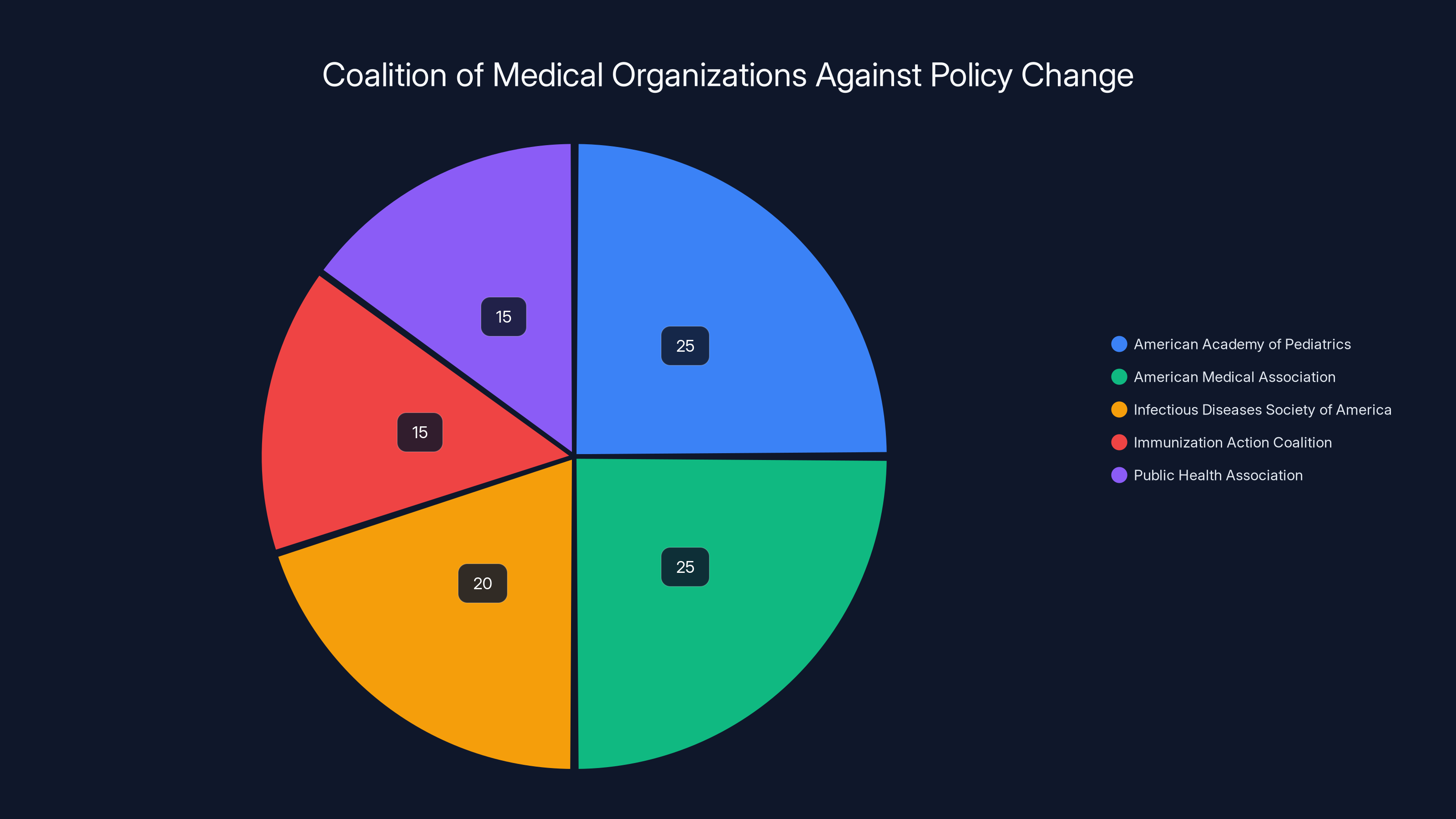
Estimated data shows a strong coalition of major medical organizations united against unilateral vaccine policy changes, emphasizing the importance of evidence-based decision-making.
The Political Calculation: Why Pharma Is Betting on Midterm Elections
Multiple executives made veiled references to waiting for the midterms. Sanofi's Hudson was most explicit: "We will have to maintain a steely focus on the long-term future of vaccines and deal with any uncertainty around vaccine coverage rates in the short-term based on misinformation, Facebook posts, and statements from the top." The implication was clear: they're treating this as a temporary political phase.
This reflects pharma's underlying theory of the situation. They believe Kennedy's anti-vaccine agenda, while currently empowered by the Trump administration, lacks broad public support. Polling suggests they might be right. When Americans are asked directly "Do you think childhood vaccines are safe?" roughly 70% say yes. Support for vaccines is durable even when anti-vaccine messaging is prominent.
Furthermore, the vaccine schedule changes will have practical consequences. As rotavirus and hepatitis A cases increase among unvaccinated children, parents will see real evidence that vaccines matter. Outbreaks are nature's most powerful counter-argument to anti-vaccine rhetoric.
If the midterms produce a shift in political power, pharma believes the vaccine schedule can be restored through the normal regulatory process. Until then, their strategy is largely defensive: maintain scientific credibility, continue funding research, support medical organizations, and wait out the political cycle.
It's a frustrating position for them. But it reflects a realistic assessment that they can't fundamentally shift the trajectory of the current administration.
Global Implications: How US Vaccine Policy Affects International Health
The United States doesn't exist in a vacuum. American vaccine policy influences global health in multiple ways.
First, the US is one of the world's largest vaccine manufacturers. American companies produce vaccines for global distribution through GAVI (the Global Alliance for Vaccines and Immunization), the World Health Organization, and bilateral aid programs. When America's vaccine schedule shifts, it creates questions about whether those vaccines are actually safe.
Kennedy's anti-vaccine messaging has already started circulating internationally. Activists in other countries are citing his statements and his policies as evidence that vaccines might not be trustworthy. This is particularly dangerous in lower-income countries where vaccine skepticism is already a challenge and vaccination rates are critically important for preventing disease outbreaks.
Second, American vaccine policy sets a precedent for other governments. If the US can unilaterally rewrite its vaccine schedule without scientific review, other countries might feel emboldened to do the same. Vaccine skepticism is a global phenomenon. If the richest nation on Earth is retreating from vaccines, it legitimizes anti-vaccine movements everywhere.
Third, the US financial contribution to global immunization programs is substantial. If American support for vaccines wanes, funding for programs that protect people in low-resource countries could decline. That would have catastrophic consequences for global health.
Public health officials at the WHO and at health ministries in other developed nations are watching the US situation with genuine alarm. What happens in America reverberates globally.

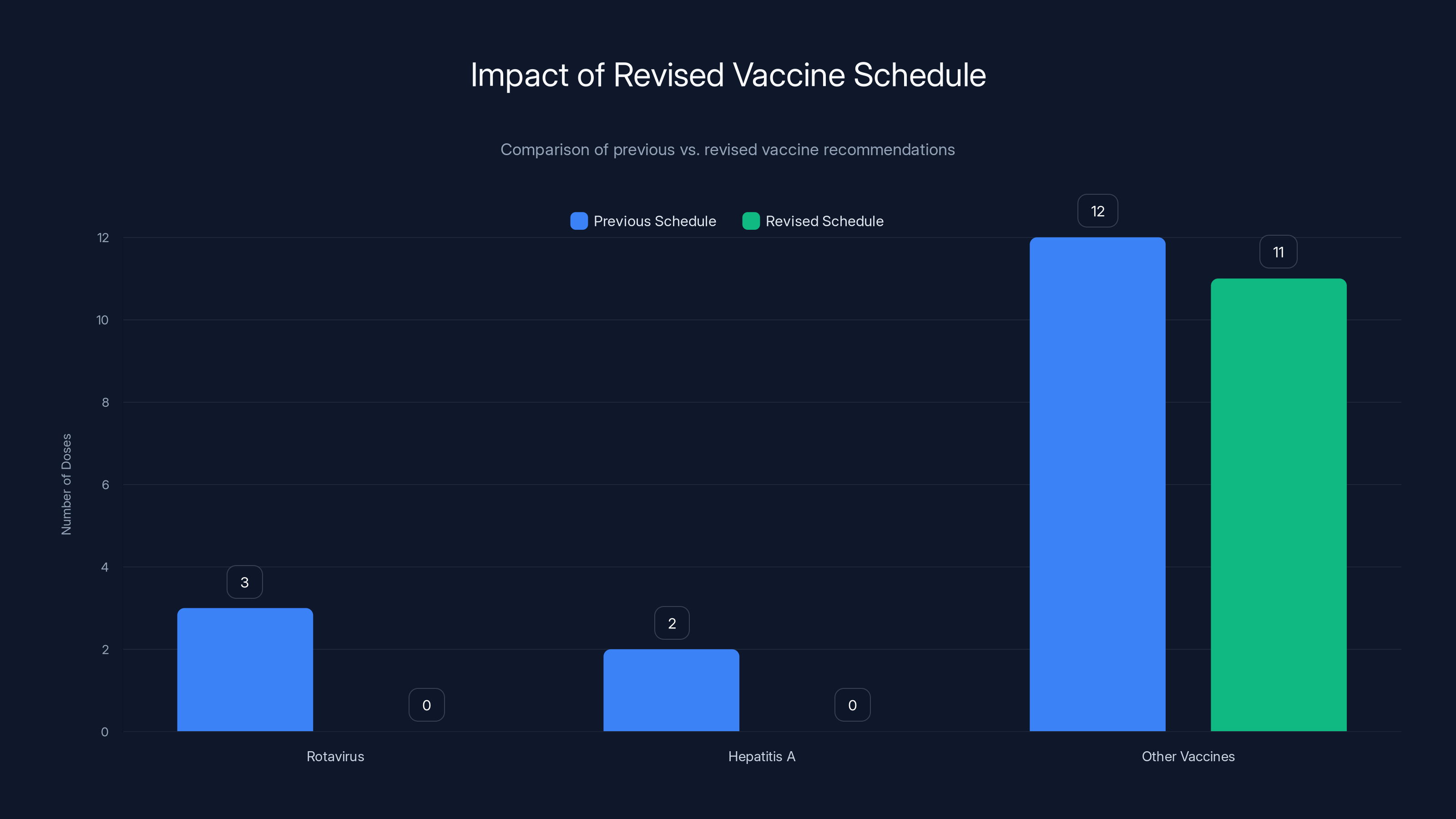
The revised schedule reduces the number of recommended vaccines by 35%, potentially increasing risk for diseases like Rotavirus and Hepatitis A. Estimated data based on typical vaccine schedules.
The Scientific Evidence: Why the Medical Community Is So Unified
One reason the pushback against Kennedy's vaccine schedule is so organized is that the scientific evidence is unusually clear-cut. Vaccines work. They're safe. The diseases they prevent are serious.
These aren't controversial claims within the scientific community. They're the consensus across decades of research involving millions of people.
Rotavirus vaccination, for example, has prevented an estimated 14 million cases of severe gastroenteritis among American children since its introduction in 2006. Before the vaccine, rotavirus sent roughly 70,000 American children to the hospital annually. After the vaccine, that number dropped by more than 80%.
Hepatitis A vaccination has similarly dramatic effects. The disease can cause severe liver dysfunction, particularly in older adults. In the decades before vaccination, thousands of Americans died from hepatitis A each year. After widespread vaccination, that number dropped to single digits.
These aren't theoretical benefits. They're documented, observed reductions in disease and death.
Kennedy claims that vaccines cause autism. This claim has been studied exhaustively. The original study that suggested such a link was fraudulent—the author lost his medical license, and the paper was retracted. Subsequent research involving millions of children has found no link between vaccines and autism. The evidence is overwhelming and consistent.
Similarly, claims that vaccines cause sudden infant death syndrome, allergies, asthma, or developmental disorders have been investigated repeatedly. The evidence doesn't support these claims.
So when the medical establishment pushes back against Kennedy, they're not defending vaccines out of financial interest or institutional habit. They're defending vaccines because the evidence supports them.
That's actually what makes pharma's position more complicated. They can argue that Kennedy's policies are scientifically unsound. That's obviously true. But they can't claim moral high ground based on pure scientific devotion, because pharma's motivations do involve profit. The pharmaceutical industry would benefit if vaccine skepticism declined.
What they can credibly argue is that the science is clear, the processes were violated, and the consequences will be serious. And those arguments have convinced not just pharma executives, but the entire medical establishment.

Corporate Interests vs. Public Health: Untangling the Complicated Motivations
Here's where the narrative gets messy. Pharma companies are criticizing Kennedy's policies. But are they motivated by genuine public health concerns or by the threat to vaccine revenue?
The answer is probably: both, in varying proportions.
Vaccines represent a significant revenue stream for pharmaceutical companies. Pfizer estimates that vaccine-related revenue will decline substantially if the childhood vaccination schedule is cut. That's not hypothetical—they've modeled it. Reduced vaccination rates mean reduced vaccine sales. It's straightforward business math.
So when Bourla criticizes Kennedy's policies, part of that criticism is self-interested. Pharma would benefit if vaccines were more widely used, and Bourla knows this.
But that doesn't make the criticism wrong. Public health and pharma profits are aligned on this issue. Both benefit if vaccines are more widely administered. The fact that pharma has a financial interest in vaccine promotion doesn't invalidate the scientific case for vaccines.
This is an important distinction. An argument can be both self-interested and correct. Burla's criticism of Kennedy might be partly motivated by profit protection, but it's also grounded in solid science. Those two things aren't mutually exclusive.
What concerns some observers is that pharma's entry into the vaccine policy debate could create a backlash. If the public sees this as "big pharma defending big pharma," it might strengthen anti-vaccine sentiment rather than weakening it. Opponents of Kennedy might have been better served by letting medical organizations carry the argument solo, without pharma's financial interests muddying the waters.
But pharma calculated that silence was worse than the reputational risk of speaking out. And given the existential threat to their industry, that calculation probably made sense.

Misinformation and Social Media: How Anti-Vaccine Messaging Spreads
Kennedy's vaccine agenda has succeeded partly because anti-vaccine misinformation is incredibly powerful on social media. A false claim about vaccines spreads faster than a true one. That's not opinion—it's documented in research on information cascades and viral content.
Anti-vaccine posts get higher engagement. They trigger emotional responses. They're simple—vaccines are presented as uniformly dangerous, a claim that's easy to understand and repeat. The true message is more complex: vaccines are remarkably safe, the diseases they prevent are serious, the benefit-to-risk ratio is overwhelmingly favorable. That's harder to communicate in a tweet or a Tik Tok.
Combine that with the fact that Kennedy himself is a prominent figure with media attention, and you have a powerful mechanism for spreading vaccine skepticism. Every press conference Kennedy holds, every interview he gives, every policy announcement he makes, generates thousands of social media posts questioning vaccine safety.
Pharma can't really compete with this through marketing. They can publish data and support medical organizations, but they're not going to out-tweet Kennedy on vaccine skepticism. The asymmetry is one reason pharma executives sound pessimistic about their ability to change the public health trajectory in the short term.
What could shift the dynamics is real-world evidence. If unvaccinated children start getting the diseases that vaccines prevent, that evidence will be visible and undeniable. An outbreak of measles or whooping cough, with children hospitalized or dying, would likely shift public opinion more effectively than any pharma campaign.
But that's an ugly way to restore vaccine confidence. It requires children to get sick before the public recognizes the value of prevention. And for public health officials, that's an unacceptable cost.
International Precedent: How Other Countries Navigate Vaccine Skepticism
The US isn't the only country dealing with vaccine skepticism. But the response to Kennedy's policies suggests that other developed nations have found better ways to handle it than just caving to anti-vaccine pressure.
Denmark, which Kennedy pointed to as an example of a country with a lower vaccine schedule, actually recommends most of the same vaccines as the US did before the cuts. The claim that other countries have successfully implemented sparse vaccine schedules is largely unsupported.
Countries like Germany, France, and the UK have experienced vaccine skepticism too, particularly around COVID vaccines. But rather than abandoning vaccination programs, these countries have invested in better communication, public transparency, and engagement with legitimate safety concerns while firmly rejecting misinformation.
The UK's approach has been particularly interesting. They've explicitly rejected calls to reduce vaccination schedules and instead focused on understanding why vaccine hesitancy exists and addressing underlying concerns. The result is that vaccine confidence in the UK is actually increasing.
There's a lesson in this international experience: capitulating to vaccine skepticism doesn't reduce it. It legitimizes it. Countries that have invested in clear communication and scientific transparency have maintained stronger public support for vaccination than countries that have wavered.
Kennedy's approach is the opposite. Rather than engaging skepticism with science, he's empowering skepticism as policy. Pharma executives believe this will backfire, that public health will suffer, and that ultimately the evidence will vindicate vaccines. But the timeline for that vindication might be measured in hospitalizations and deaths.

The Road Ahead: Scenarios and Predictions for Vaccine Policy
What happens next? There are several plausible scenarios.
Scenario 1: Legal Challenges Succeed. The American Academy of Pediatrics and other organizations prevail in court, establishing that Kennedy exceeded his authority. The vaccine schedule is restored through judicial intervention. Timeline: 12-24 months. This seems possible based on administrative law principles, but it's uncertain because the Trump appointees sitting on federal courts might view Kennedy's authority more generously.
Scenario 2: Outbreaks Drive Public Opinion Shift. Rotavirus or hepatitis A cases increase noticeably among unvaccinated children. Parents observe the consequences and demand vaccines. Public pressure forces a reversal of the schedule changes. Timeline: 6-18 months. This is depressingly realistic—disease outbreaks are often the most powerful argument for vaccines.
Scenario 3: Political Change. The 2026 midterm elections produce a shift in power, and a new administration restores vaccine confidence and the standard schedule. Timeline: 12+ months until implementation. This aligns with what pharma executives are betting on.
Scenario 4: Persistent Damage. Kennedy's policies survive legal challenges, generate sustained anti-vaccine sentiment, and establish a precedent for questioning other public health policies. Vaccination rates decline persistently. Disease incidence increases. The US becomes a cautionary tale about what happens when ideology overrides science in public health. Timeline: Ongoing.
Each scenario has different implications for pharma, for public health, and for the scientific integrity of health policy. But all of them underscore that this moment represents a genuine inflection point in American public health policy.

The Broader Threat: What Kennedy's Vaccine Crusade Signals About Medical Policy
Pharma executives aren't just worried about vaccines. They're worried about what this precedent means for other medications and medical interventions.
Bourla made this explicit: "Today it may be childhood vaccines or mRNA, but tomorrow it's everything." His concern is that once the norm of scientific review is broken, it becomes easier to break it again. If Kennedy can bypass the standard vaccine review process, what prevents him from doing the same for cancer drugs? For insulin? For antibiotics?
The threat is that Kennedy's anti-vaccine agenda is the beginning of a broader assault on evidence-based medicine. That might sound paranoid, but Kennedy's track record suggests it's not entirely unfounded. He's expressed skepticism about a remarkably broad range of medical interventions, from mercury in vaccines to fluoride in water to the official HIV origin narrative.
For an industry dependent on evidence-based medicine and regulatory trust, this is existential. Pharma needs the world to believe that drugs are safe because they've been tested and evaluated by credible scientists. If that belief erodes, if vaccines can be rejected without scientific proof, then any drug is vulnerable to attack.
So pharma's pushback against Kennedy isn't just about protecting vaccine revenue. It's about protecting the institutional framework that allows modern medicine to function.
That's why the stakes feel so high, even to executives accustomed to high-stakes regulatory battles.

The Role of Scientific Integrity: Why Process Matters as Much as Content
One element that deserves emphasis: much of pharma's criticism isn't really about vaccines specifically. It's about the decision-making process.
If Kennedy had come to the ACIP committee, presented evidence, engaged in peer review, and argued that the vaccine schedule should be modified, that would be legitimate. Even if the committee ultimately disagreed with him, the process would be credible.
But he didn't do that. He bypassed the process entirely. And that's what triggers the institutional response from pharma, from medical organizations, from the scientific community.
This gets at something important: science depends on process. The reason we trust the scientific consensus about vaccines isn't just because individual studies are well-designed. It's because the consensus has been reached through systematic review, peer critique, and repeated validation across independent research groups.
Kennedy's approach—announce a conclusion, don't ask for scientific input, declare it policy—is the antithesis of scientific process. From pharma's perspective, this represents a threat to the entire infrastructure of evidence-based medicine.
FAQ
What is the childhood vaccine schedule and why was it changed?
The childhood vaccine schedule is a list of recommended vaccinations for children from birth through age 18, established by health authorities to protect against serious diseases. Kennedy's administration reduced recommended routine vaccines from 17 to 11, eliminating protection against diseases like rotavirus and hepatitis A, without undergoing the standard scientific review process that typically takes 6-12 months.
Who is Robert F. Kennedy Jr. and what are his credentials in medicine?
Robert F. Kennedy Jr. is an environmental lawyer with no medical, epidemiological, or public health degree. He has worked in litigation against vaccine manufacturers and has profited from vaccine-injury lawsuits, which critics argue represents a conflict of interest in his role as Health Secretary.
Why did pharmaceutical executives criticize the vaccine policy changes?
Pharmaceutical executives criticized the changes because they violated the scientific review process, contradicted medical evidence, lacked justification, and threatened public health outcomes. Additionally, they worried about legal litigation risks, declining vaccination rates, and the precedent of bypassing scientific procedures for major health policies.
What do other countries' vaccine schedules look like compared to the US?
Of 20 peer nations analyzed, the US after the cuts recommends significantly fewer vaccines than almost all comparable countries. Only Denmark has a similarly sparse schedule. Countries like Germany, Canada, Australia, France, Italy, Spain, Sweden, Norway, and Japan all recommend more vaccines than the newly revised US schedule.
What are the potential health consequences of reducing childhood vaccinations?
Reducing vaccinations increases risk of disease outbreaks. Rotavirus previously caused 70,000 hospitalizations annually in the US before the vaccine; hepatitis A can cause severe liver dysfunction and death. Lower vaccination rates are expected to increase childhood hospitalizations and deaths from preventable diseases by thousands annually.
Are there legal challenges being mounted against the vaccine schedule changes?
Yes, the American Academy of Pediatrics and other medical organizations have announced preparation of formal legal challenges. These argue that Kennedy exceeded his authority by bypassing the established scientific review process and administrative procedures required for such changes.
What is the timeline for when the vaccine policy situation might change?
Pharmaceutical executives suggest the main timeline is the midterm elections (2026), implying they view this as a temporary political phenomenon. Legal challenges could take 12-24 months to resolve. Real-world consequences like disease outbreaks could also shift public opinion within 6-18 months.
Conclusion: The Inflection Point for Science-Based Health Policy
What happened at the J. P. Morgan Healthcare Conference in January 2025 marked a significant shift. For the first time, the pharmaceutical industry openly and directly challenged a sitting administration's health policy. They didn't couch their criticism in careful language or hedge their bets. They called it what they saw: an assault on science without merit.
That willingness to speak openly came at a cost. Pharma is exposing itself to criticism that it's defending its own interests rather than genuinely concerned about public health. There's truth to that. But there's also truth to the fact that science-based medicine and pharma's commercial interests are currently aligned on vaccines.
The broader story here is about the intersection of politics, science, and public health policy. Kennedy's approach represents a fundamental challenge to evidence-based medicine: the idea that major health decisions should be made through transparent scientific review rather than political ideology. That's not a small thing. It's foundational to how modern medicine works.
Pharma executives recognize this. Doctors recognize this. The international health community recognizes this. And that's why the response has been so immediate and organized, despite the political power Kennedy wields.
What happens next will determine whether the US maintains science-based health policy or shifts to a more ideologically-driven approach. The stakes—measured in hospitalized children and preventable deaths—are enormous.
For now, the battle continues. Legal teams prepare challenges. Medical organizations coordinate opposition. Pharmaceutical executives wait for political winds to shift. And unvaccinated children remain vulnerable to diseases that vaccines can prevent.
The fundamental question persists: In America's health system, does science or ideology guide policy? Kennedy's vaccine agenda is answering that question in real time. And whether the answer ultimately comes through courts, through disease outbreaks, or through electoral change remains to be seen.
What's certain is that this moment will be remembered as consequential—either as the moment when evidence-based medicine prevailed against political pressure, or as the beginning of its decline.

Key Takeaways
- Pharmaceutical executives publicly criticized RFK Jr.'s vaccine schedule reduction from 17 to 11 vaccines, marking unprecedented pushback against Trump administration health policy
- The vaccine schedule changes bypassed all standard scientific review processes, violating the 6-12 month deliberative procedures that normally govern such decisions
- The United States now ranks among the lowest in vaccine recommendations compared to peer nations, contradicting Kennedy's claim of international alignment
- Major medical organizations including the American Academy of Pediatrics are preparing legal challenges, arguing the health secretary exceeded his authority
- Pharmaceutical executives believe this situation is temporary and are strategically waiting for the 2026 midterm elections to shift political power and restore vaccine confidence
![Pharma Execs Strike Back: RFK Jr.'s Vaccine Agenda Under Fire [2025]](https://tryrunable.com/blog/pharma-execs-strike-back-rfk-jr-s-vaccine-agenda-under-fire-/image-1-1768520153917.jpg)



